Pediatric Patients Undergoing Elective Surgeries Below the Umbilicus: Comparative Study of Caudal Bupivacaine (0.25%) and Caudal Bupivacaine (0.25%) with Ketamine
A B S T R A C T
Background: Caudal block has the potential advantage that, by adding other drugs to the local anaesthetic agent, the duration and effectiveness of the block may be extended. Peripheral nerve blocks and caudal anaesthesia are very benign, nonetheless inordinate attention is compulsory to evade side effects.
Aim and objectives: We aimed at this study to compare total postoperative analgesic requirement, anaesthetic, analgesic and sedation qualities. Hemodynamic changes, motor block, adverse effect, and parents’ satisfaction in children who received caudal bupivacaine only versus caudal bupivacaine with ketamine in paediatric patients undergoing surgery below the level of the umbilicus.
Methods: Prospective randomized double blind controlled clinical trial conduced at operation room in University Hospital in Faculty of Medicine, October 6 University. Sixty children scheduled for elective surgery below umbilicus were randomly allocated to either: Group A (30 patients) includes the children who take saline caudal bupivacaine with dose of 1 ml/kg, afterward initiation of overall anaesthesia or Group B (30 patients) who following the administration of general anaesthesia, receives caudal bupivacaine 0.25 % in a dose of 1 ml/kg and caudal ketamine preservative free in a dose of 0.5 mg/kg. Hemodynamic alterations, parent satisfaction, postoperative analgesia and sedation characteristics, and side effects were noted.
Results: The studied groups showed no statically significant difference regarding demographic data. Motor block statistically was significantly lower in ketamine group. Anaesthesia quality statistically was significantly higher in ketamine group. Regarding hemodynamic state, mean arterial blood pressure (MPA) and heart rate showed a statistically significant difference during and up to 30 minute postoperative (P<0.001), and oxygen saturation showed no statistically significant difference during and after surgery (P>0.05). Sedation score was higher in ketamine group, were lower in ketamine group all were statistically significant. Side effects statistically were non-significantly but less frequent in ketamine group. Total 24-hours analgesia dose statistically was significantly lesser in ketamine group. Parent’s satisfaction statistically was suggestively better in ketamine group.
Conclusion: Amalgamation therapy of ketamine with bupivacaine is enhanced decision for post-operative pain controller in children enduring surgery below the umbilical. It increased the duration of analgesia and abridged the necessity for post-operative analgesic supplementation as well.
Keywords
Caudal Bupivacaine, ketamine, anaesthesia and analgesia quality in pediatric surgeries, postoperative pain
Introduction
Post-operative pain is typically undertreated in this oldness range since it is difficult to measure pain in the paediatric population. Children's pain has a strong emotional component; thus, pain alleviation is required [1]. Each person has a different experience of pain, which is a complicated phenomenon with a lot of qualities like strength, superiority, time course, and affects. Due to the effective delineation of pain's requirement for self-report, pain expert by children is habitually unnoticed or underreported [2].
Compared to using general anaesthesia alone, regional methods and general anaesthesia together depict children of all ages to fewer intravenous and inhalational anaesthetics and analgesics, keeping them almost free of motion sickness, heaving, or needless drowsiness. Children and parents both appreciate the benefits of recovering abundantly conscious, being up to drink right away afterward surgery, and not had any respiratory issues even afterward a lengthy procedure [3]. Caudal block has the potential advantage that, by adding other drugs to the local anaesthetic agent, the duration and effectiveness of the block may be extended. Drugs used to achieve this have included morphine, clonidine, ketamine and midazolam [4].
Marginal nerve blocks and caudal anaesthesia are very benign, nonetheless prodigious attentiveness is continuously obligatory to evade side effects. Safety be contingent seriously on the adequate exercise of pediatric anaesthesiologists. The well-trained pediatric anaesthesiologist stabs to evade perilous protocols of application of regional anaesthetics and is permanently set to treat risky side effects [5].
Ketamine is a non-competitive blocker and hypothesized to avert or converse essential sensitization and subsequently diminish postoperative pain; in addition, it has a peripheral analgesic outcome. The practise of ketamine permeation in children undertaking adenotonsillectomy has been found to provide side-effect-free pain relief up to 24 hours following surgery. The primary intention of this study was to improve analgesic, anaesthetic and sedation qualities, secondary to decrease total post-operative analgesic requirement and side effect in children underwent elective surgeries below umbilicus [6].
Materials and Methods
After endorsement of medical ethics committee of October 6 University, the children’s parents were well-versed by the protocol of the study and a written consent was attained from all parents, the study was registered prospectively in Clinical Trials Registry (NCT05444036). Inclusion criteria: All children below five years old with American society of anaesthesiologists physical status (ASA) I or II programmed for non-compulsory surgery below umbilicus were adequate to participate into the study.
Exclusion criteria: Those children having allergy or sensitivity to bupivacaine and ketamine or those having any contraindication to caudal injection, i.e., infection at the site, bleeding disorder, and caudal vertebral anomalies were excluded.
Sample size: sample size is 30 patients in each group calculated using the following formula

Preoperative valuation of the patients encompassed: medical history, physical examination and laboratory investigations, the fathers were tutored to preserve the children nil orally up to 6 hr. afore surgery, and oral clear fluid were allowable only up to 3 hr. afore surgery. Visual analogue scale (VAS) was explained to child parent to point to the position on the line between faces to indicate how much pain they might feel [8]. In this system the total scores range from 0 to 10 based on measuring the distance in millimetres from the left end bar to mark made by the child on the 10 cm line anchored by happy face (no pain) to sad faces (sever pain) with a higher score indicating more severe pain.
Consistent with their consigned groups, each child received a caudal injection. Once the operation was over, the muscle relaxant was overturned with atropine 0.03 mg/kg and neostigmine 0.05 mg/kg intravenously, and the patient was extubated when unprompted airing was sufficient. The anaesthesia was upheld with isoflurane 1-1.5 MAC, 100 % oxygen, and rocuronium 0.1 mg/kg when compulsory. Children were sent to the post-anaesthesia care unit (PACU), wherever they underwent a 24-hour postoperative stay after being observed in the recovery room for up to an hour.
0.2 mg/kg of ephedrine was administered intravenously to treat intraoperative hypotension (systolic blood pressure 75 mmHg), 0.02 mg/kg of atropine was administered intravenously to treat bradycardia (heart rate 60 beats/min), and an oxygen face mask was administered to treat hypoxemia (decrease in oxygen saturation 90%). postoperative nausea and vomiting were treated by 4mg of intravenous Cortigen B6. Duration of analgesia is demarcated as the interval since the drug's caudal injection and first time child complain from pain and received analgesic. The length of analgesia was measured in 24-hour increments if it wasn't absolutely necessary within the 24-hour observation period.
Analgesic drug was set to children once their VAS extended four or more and entail paracetamol 15 mg/kg by mouth every 4 hr. Recording the time of any side outcomes timing of micturition and any sign of nightmares, hallucinations, or odd actions or any extra side outcome were recorded. The total requirement of post-operative analgesia in the 24-h period were recorded.
Motor blocks were assessed by Bromage scale [9]:
0 - Capable of lifting extended legs with full knee and foot flexion.
1 - Talented of bending knees and feet but incapable to lift protracted legs
2 - Knee flexion is impossible while foot flexion is possible
After completion of surgery patient parent satisfaction was recorded by using numeric scale as follows: excellent (4): no complaint, good (3): patient complaint from minor pain but no need for analgesia, fair (2): patient complaint from moderate pain and need analgesics, failed (1): patient cannot tolerate, and child take analgesic drug shortly after recovery.
Sedation score was used to evaluate post-operative sedation: 1 represents being fully awake, 2 represents being awake but drowsy, 3 represents being asleep but still responding to commands, 4 represents being insensible but responding to perceptible stimulus, and 5 represents being asleep but not responding to any stimulus [10]. All drugs injected by anaesthesiologists blind to our study, and data observed and recorded were done by another blinded anaesthesiologists to the study.
Statistical Analysis
The collected data were implicit, tabularised, and scrutinised using IBM SPSS statistics (Statistical Package for Social Sciences) software version 28.0, IBM Corp., Chicago, USA, 2021. Numerical statistics verified using Shapiro-Wilk test, then if normally distributed described as Mean±SD (standard deviation), then linked using independent t-test. Qualitative data designated as number and percentage and compared using Chi square test and Fisher’s exact test for variables with small, estimated numbers. The level of significance was taken at P value < 0.050 was significant.
Results
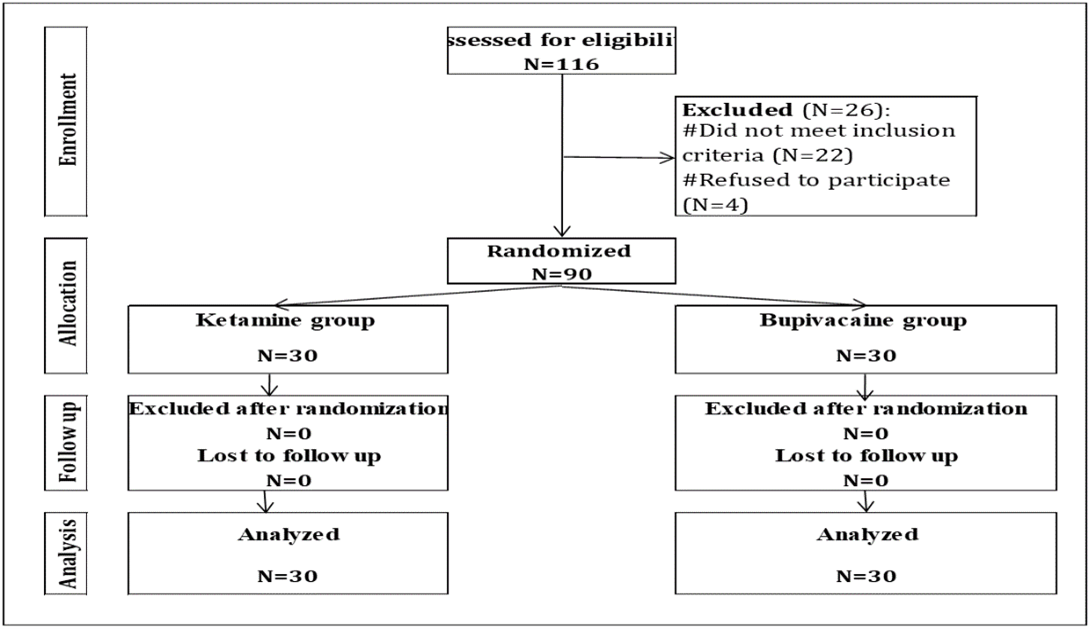
30 children undergoing surgery below umbilicus in the period from September 2018- June 2019 in October six university hospital was alienated to two groups. All 60 patients enrolled in the study as shown in (Figure 1).
Table 1 shows that: No significant statistical differences between the studied groups regarding age, sex, and weight and surgery type. Table 2 displays that: No significant statistical difference between the studied groups regarding operation duration. Bromage measure for motor block statistically was significantly low-grade in ketamine group. Anaesthesia value statistically was significantly higher in ketamine group.
Table 1: Comparison according to demographic characteristics.
|
Variables |
Ketamine (N=30) |
Bupivacaine (N=30) |
p-value |
|
|
Age
(years), Mean±SD |
3.1±1.5 |
2.8±1.2 |
^0.393 |
|
|
Sex (N,
%) |
Male |
11
(36.7%) |
14
(46.7%) |
#0.432 |
|
Female |
19
(63.3%) |
16
(53.3%) |
||
|
Weight
(kg), Mean±SD |
17.4±3.8 |
17.1±2.8 |
^0.718 |
|
|
Surgery
type (N,
%) |
Hernia
repair |
17
(56.7%) |
19
(63.3%) |
§0.703 |
|
Hydrocele |
5
(16.7%) |
6
(20.0%) |
||
|
Orthopedic
in lower extremities |
5
(16.7%) |
2
(6.7%) |
||
|
Other
surgeries |
3
(10.0%) |
3
(10.0%) |
||
^Independent
t-test; #Chi square test; §Fisher's exact test.
Figure 1: CONSORT of the deliberated cases.
Table 2: Surgical time, intraoperative motor block, and
anaesthetic value comparison.
|
Ketamine (N=30) |
Bupivacaine (N=30) |
P
value |
Ketamine's
impact in respect to bupivacaine |
||||
|
Mean±SD
|
95%
CI |
||||||
|
Operation
time (min), Mean±SD |
62.4±11.7 |
62.8±13.4 |
^0.894 |
-0.4±3.3 |
-6.9–6.1 |
||
|
|
|
|
|
RR |
95%
CI |
||
|
Bromage
scale |
0 |
24
(80.0%) |
16
(53.3%) |
§0.031* |
1.50 |
1.03–2.19 |
|
|
1 |
6
(20.0%) |
9
(30.0%) |
Reference |
||||
|
2 |
0
(0.0%) |
5
(16.7%) |
|||||
|
Anaesthesia
value |
Excellent |
16
(53.3%) |
7
(23.3%) |
#0.017* |
2.29 |
1.10–4.74 |
|
|
Good |
12
(40.0%) |
14
(46.7%) |
Reference |
||||
|
Moderate |
2
(6.7%) |
9
(30.0%) |
|||||
^Independent
t-test; §Fisher's Exact test; #Chi square test; *Significant; RR: Relative risk;
CI: Confidence interval.
Figure 2 shows that: Heart rate in both groups was increasing in ketamine group from baseline till minute-15 postoperatively then began to decrease. Blood pressure was rising in the group ketamine beginning the baseline throughout the procedure before it started to fall postoperatively, while in control group was decreasing in from zero throughout operation then instigated to fall post-operatively as publicized in (Figure 3). Heart rate and mean blood pressure statistically were significantly higher in ketamine group beginning from intraoperative minute-5 throughout operative duration and till postoperative minute-30, the maximum gab between the studied groups was at operation end. No statistically significant variances amid the studied groups concerning intraoperative and postoperative oxygen saturation as revealed in (Figure 4) (Table 3).
Figure 2: Evaluation regarding heart rate.
IP: Intraoperative. PO: Postoperative. M: Minute. *Significant
Figure 3: Evaluation regarding mean blood pressure.
IP: Intraoperative. PO: Postoperative. M: Minute. *Significant
Figure 4: Evaluation regarding oxygen saturation.
IP: Intraoperative. PO: Postoperative. M: Minute. *Significant
Table 3: The means of heart rate, mean arterial pressure and
peripheral oxygen saturation at various times of measurements in the two
studied groups.
|
Time |
K/B (n=30) |
B/S (n=30) |
^P-value |
Effect
of ketamine relative to Bupivacaine |
||
|
Mean±SEM
|
95%
CI |
|||||
|
Heart rate (beat/minute) |
||||||
|
Baseline |
74.3±2.9 |
73.4±3.5 |
0.271 |
0.9±0.8 |
-0.7–2.6 |
|
|
IP, minute-5 |
81.1±2.7 |
76.0±3.6 |
<0.001* |
5.1±0.8 |
3.4–6.7 |
|
|
IP,
minute-10 |
89.2±2.3 |
80.7±3.1 |
<0.001* |
8.5±0.7 |
7.1–9.9 |
|
|
IP, minute-15 |
96.9±2.5 |
83.1±3.4 |
<0.001* |
13.7±0.8 |
12.2–15.3 |
|
|
IP,
minute-30 |
101.3±2.5 |
84.8±3.0 |
<0.001* |
16.5±0.7 |
15.1–17.9 |
|
|
IP, operation end |
105.5±3.4 |
85.7±4.1 |
<0.001* |
19.9±1.0 |
17.9–21.8 |
|
|
PO,
minute-5 |
106.1±2.9 |
86.9±3.3 |
<0.001* |
19.1±0.8 |
17.5–20.7 |
|
|
PO, minute-15 |
106.4±2.8 |
86.6±3.0 |
<0.001* |
19.8±0.8 |
18.3–21.3 |
|
|
PO,
minute-30 |
103.1±2.9 |
84.4±3.1 |
<0.001* |
18.7±0.8 |
17.1–20.3 |
|
|
Mean blood pressure (mmHg) |
||||||
|
Baseline |
71.9±3.2 |
71.3±2.5 |
0.447 |
0.6±0.7 |
-0.9–2.0 |
|
|
IP, minute-5 |
81.1±3.7 |
70.4±2.7 |
<0.001* |
10.8±0.8 |
9.1–12.4 |
|
|
IP,
minute-10 |
88.9±3.3 |
66.7±2.7 |
<0.001* |
22.2±0.8 |
20.6–23.8 |
|
|
IP, minute-15 |
95.3±3.3 |
66.8±2.7 |
<0.001* |
28.5±0.8 |
27.0–30.0 |
|
|
IP,
minute-30 |
99.5±3.6 |
65.7±3.3 |
<0.001* |
33.8±0.9 |
32.0–35.6 |
|
|
IP, operation end |
103.4±2.5 |
64.6±3.5 |
<0.001* |
38.8±0.8 |
37.3–50.4 |
|
|
PO,
minute-5 |
104.8±4.3 |
68.9±3.6 |
<0.001* |
36.0±1.0 |
33.9–38.0 |
|
|
PO, minute-15 |
103.4±3.0 |
71.4±2.9 |
<0.001* |
32.0±0.8 |
30.5–33.5 |
|
|
PO,
minute-30 |
102.8±4.3 |
75.5±3.6 |
<0.001* |
27.4±1.0 |
25.3–29.4 |
|
|
Oxygen saturation (%) |
||||||
|
Baseline |
99.5±0.5 |
99.6±0.5 |
0.447 |
-0.1±0.1 |
-0.4–0.2 |
|
|
IP, minute-5 |
99.0±0.6 |
99.1±0.6 |
0.521 |
-0.1±0.2 |
-0.4–0.2 |
|
|
IP,
minute-10 |
99.2±0.6 |
99.3±0.5 |
0.451 |
-0.1±0.1 |
-0.4–0.2 |
|
|
IP, minute-15 |
99.3±0.5 |
99.1±0.5 |
0.142 |
0.2±0.1 |
-0.1–0.5 |
|
|
IP,
minute-30 |
99.1±0.3 |
99.0±0.2 |
0.168 |
0.1±0.1 |
-0.1–0.2 |
|
|
IP, operation end |
99.0±0.5 |
99.0±0.6 |
0.999 |
0.0±0.1 |
-0.3–0.3 |
|
|
PO,
minute-5 |
99.3±0.6 |
99.3±0.7 |
0.999 |
0.0±0.2 |
-0.3–0.3 |
|
|
PO, minute-15 |
99.3±0.5 |
99.1±0.5 |
0.147 |
0.2±0.1 |
-0.1–0.5 |
|
|
PO,
minute-30 |
99.4±0.5 |
99.2±0.5 |
0.203 |
0.2±0.1 |
-0.1–0.4 |
|
Data
presented as Mean±SD; IP: Intraoperative; SE: Standard error; CI: Confidence
interval; ^Independent t-test; *Significant.
Table 4 demonstrates that: Sedation score was greater in the ketamine group, period to first micturition and period to impulsive the opening of eye were both substantially slower in the ketamine group. The ketamine group experienced less frequent but statistically non-significant nausea, vomiting, and headaches.
Table 4: Post-operative sedation score, period of micturition
and adjacent effects assessment.
|
Variables
|
Ketamine (N=30) |
Bupivacaine (N=30) |
t-test |
Outcome
of ketamine respect to Bupivacaine |
|
|
Mean±SD
|
95%
CI |
||||
|
Sedation
score, Mean±SD |
3.6±1.0 |
2.6±1.0 |
<0.001* |
-1.0±0.3 |
-1.5–-0.5 |
|
Time
to first micturition (hours), Mean±SD |
16.6±2.1 |
24.5±3.7 |
<0.001* |
-7.8±0.8 |
-9.4–-6.3 |
|
Time
to spontaneous eye opening (minutes), Mean±SD |
3.4±1.2 |
3.0±1.1 |
0.208 |
0.4±0.3 |
-0.2–0.9 |
|
|
|
|
|
RR |
95%
CI |
|
Nausea,
(n, %) |
2 (6.7%) |
7
(23.3%) |
§0.154 |
0.29 |
0.06-1.26 |
|
Vomiting,
(n, %) |
2
(6.6%) |
4
(13.3%) |
§0.512 |
0.34 |
0.05-4.04 |
|
Headache,
(n, %) |
4
(13.3%) |
8
(26.6%) |
#0.063 |
0.43 |
0.11-1.32 |
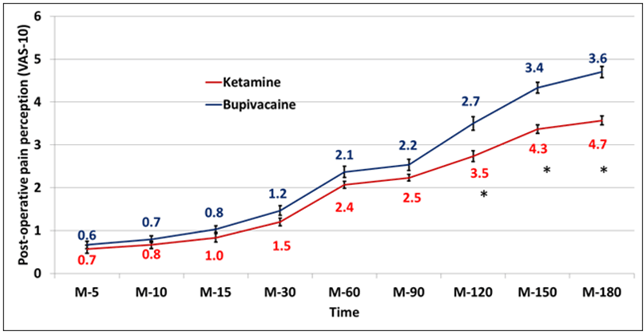
According to (Table 5 and Figure 5), the ketamine group experienced less postoperative discomfort, with differences becoming statistically significant between minutes 120 and 180. Statistics show that the ketamine group had a considerably longer time to the initial rescue analgesia. Statistics showed that the ketamine group had a considerably lower 24-hour analgesia dose overall. Statistics showed that the ketamine group had much higher parent satisfaction. Figure 6 shows that: Rate of need to first rescue analgesia statistically was significantly lower in ketamine group.
Table 5: Evaluation of parents' satisfaction with analgesia,
postoperative pain perception, and the need for analgesia.
|
Time
|
Ketamine (N=30) |
Bupivacaine (N=30) |
^ t-test |
Outcome
of ketamine respect to Bupivacaine |
|||
|
Mean±SD
|
Range
|
||||||
|
Post-operative
pain perception (VAS-10), Mean±SD |
|||||||
|
Minute-5 |
0.6±0.32 |
0.7±0.5 |
0.434 |
-0.1±0.11 |
-0.4–0.21 |
||
|
Minute-10 |
0.7±0.23 |
0.8±0.4 |
0.250 |
-0.1±0.11 |
-0.4–0.11 |
||
|
Minute-15 |
0.8±0.42 |
1.0±0.4 |
0.109 |
-0.2±0.1 |
-0.4–0.0 |
||
|
Minute-30 |
1.2±0.25 |
1.5±0.6 |
0.071 |
-0.3±0.1 |
-0.6–0.0 |
||
|
Minute-60 |
2.1±0.15 |
2.4±0.7 |
0.058 |
-0.3±0.2 |
-0.6–0.0 |
||
|
Minute-90 |
2.2±0.14 |
2.5±0.7 |
0.059 |
-0.3±0.21 |
-0.6–0.0 |
||
|
Minute-120 |
2.6±0.80 |
3.15±0.91 |
<0.01* |
-0.8±0.21 |
-1.2–-0.41 |
||
|
Minute-150 |
3.5±0.51 |
4.13±0.71 |
<0.01* |
-1.0±0.21 |
-1.3–-0.61 |
||
|
Minute-180 |
3.7±0.50 |
4.17±0.71 |
<0.01* |
-1.1±0.21 |
-1.5–-0.81 |
||
|
Analgesia
prerequisite, Mean±SD |
|||||||
|
Time
to first rescue analgesia (minutes) |
157.0±26.9 |
122.0±35.2 |
<0.001* |
35.0±8.1 |
18.8–51.2 |
||
|
Total
24-hours analgesia dose (gm) |
0.9±0.2 |
1.2±0.3 |
<0.001* |
-0.3±0.1 |
-0.5–-0.2 |
||
|
Parent’s
satisfaction, (n, %) |
|||||||
|
Grades |
|
|
|
RR |
95%
CI |
||
|
Fair |
2
(6.71%) |
17
(56.7%) |
#<0.001* |
0.12 |
0.03–0.47 |
||
|
Good |
7
(23.31%) |
8
(26.7%) |
Reference |
||||
|
Very
good |
10
(33.3%) |
4
(13.3%) |
|||||
|
Excellent |
11
(36.7%) |
1
(3.3%) |
|||||
^Independent
t-test; #Chi square test; *Significant; RR: Relative risk; CI: Confidence
interval.
Figure 5: Evaluation concerning post-operative pain awareness.
IP: Intraoperative; PO: Postoperative; M: Minute; *Significant.
Figure 6: Kaplan Meier Curve for first rescue analgesia rate.
Discussion
The most stressful warning sign practised by patients enduring any chief surgery is the post-operative pain, it persuades a innumerable effects comprising a metabolic, hormonal, cardio and respiratory response that might disturb the outcome post operatively [11]. Children are at an increased risk of this hazard, as they do not express pain like adults. Regardless of the cruelty of their pain, children get much less medicine because using opioid analgesics continuously increases the risk of drowsiness and respiratory depression [12]. Alpha 2 Adrenergic receptor agonists could prolong the duration of action of bupivacaine and improve the quality of analgesia, by causing local vasoconstriction and increasing the potassium conductance in A , D and C fibres [4]. Additionally, they may boost the possessions of confined anaesthetics by diffusing into cerebrospinal fluid or systemically absorbing them to reach alpha 2 receptors in the apparent laminae of the spinal cord and brainstem, or by circuitously triggering vertebral cholinergic neurones [13].
Caudal spinal anaesthesia is unique of the greatest communal regional techniques used in the paediatric age group. It is commended for most infra-umbilical surgical trials similar herniorrhaphy, manoeuvres on the urogenital tract, and rectum and orthopaedic trials on the minor extremities [14]. The finite and brief duration of the single-shot caudal blockage is a drawback that limits its usefulness as a postoperative painkiller. Only 4-6 hours of analgesia are offered by even long-acting local anaesthetic medications like bupivacaine. Accordingly, scientists are continuously observing for the best adjuvant to encompass the effects of painlessness [15].
This study compared the analgesic, anaesthetic, and sedative effects of caudal block with bupivacaine versus caudal block with ketamine in paediatric patients undergoing surgery below the level of the umbilicus. It also compared the total amount of postoperative analgesia needed, hemodynamic changes, motor block, parents' satisfaction, and side effects. Post-operative pain perception was reduced in the ketamine group, according to the study's findings. The changes were statistically significant from minute 120 to minute 180. Time to first rescue analgesia statistically was significantly longer in ketamine group. Total 24-hours analgesia dose statistically was meaningfully lower in ketamine group. Parent’s satisfaction statistically was expressively better in group ketamine.
In this work, upon comparison of the two studied groups regarding bromage-scale in group ketamine was significantly lesser than bupivacaine. In contrast, Shafqat et al. compared 2 groups of patients and established that bromage-scale (post-operative) of both the groups at 1, 4, 6, 12 and 24 hours were not statistically significant difference at any of the hour among the groups. This may be due to different types of surgeries conducted on their participants [16].
Kaur et al. steered a study aimed at evaluating the effectiveness and safety of bupivacaine alone against bupivacaine and ketamine for post-operative analgesia in paediatric patients that had an infraumbilical surgery. They concluded that addition of ketamine 0.5 mg/kg to caudal bupivacaine 0.25% in a dose of 1 ml/kg significantly prolonged the postoperative analgesia and diminution rescue analgesic dose needed equated by administrating of caudal bupivacaine 0.25% in a dose of 1 ml/kg alone. Their conclusion support our study [17].
In addition, Farrag et al. settled that ketamine group delivers longer duration of post-operative analgesia as equated to magnesium sulphate group when likening bupivacaine 0.25 % plus 0.5mg per kg. However, in our study, we compared ketamine combination [3]. Supporting our research with bupivacaine, Naz et al. (2020) noted a pain-free duration of 5.7 ± 0.81 hours, whereas the addition of ketamine lengthened the mean of analgesia duration to 9.3±1.65 hrs [5].
A study steered by Shafqat E et al. on 80 pediatric patient who settled that children established with Ketamine 0.5 mg/kg and bupivacaine 0.25% in a dose of 1 ml/kg experienced prolonged duration of postoperative analgesia to a significant range in comparison with bupivacaine 25% of 1ml/kg alone. Their study results goes with our study [17]. In contrast, Khan and Anand steered a study in Pakistan pointed at equating the side effect profile and the duration of action for tramadol-bupivacaine and Ketamine-bupivacaine, as post-operative pain management in the paediatric age group. Caudal tramadol with bupivacaine formed meaningfully augmented the postoperative analgesia [2].
In this study, when investigating side effects, ketamine group was significantly lower than bupivacaine group. To add to our study, in a research by Abelard et al., only 1 patient in the caudal group ketamine and 4 patients (20%) in the caudal bupivacaine-ketamine group reported postoperative nausea and vomiting [20].
Conclusion
Amalgamation treatment of ketamine with bupivacaine is superior alternative for post-operative pain controller in youngsters undertaking below umbilical surgery. It augmented the duration of analgesia and lessen the need for post-operative analgesic supplementation as well.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 27, Jun 2022Accepted: Mon 11, Jul 2022
Published: Tue 26, Jul 2022
Copyright
© 2023 Nirvana Ahmed Elshalakany. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ACR.2022.02.03
Author Info
Corresponding Author
Nirvana Ahmed ElshalakanyAnaesthesia and Intensive Care Unit, Faculty of Medicine, October 6 University, Cairo, Egypt
Figures & Tables
Table 1: Comparison according to demographic characteristics.
|
Variables |
Ketamine (N=30) |
Bupivacaine (N=30) |
p-value |
|
|
Age
(years), Mean±SD |
3.1±1.5 |
2.8±1.2 |
^0.393 |
|
|
Sex (N,
%) |
Male |
11
(36.7%) |
14
(46.7%) |
#0.432 |
|
Female |
19
(63.3%) |
16
(53.3%) |
||
|
Weight
(kg), Mean±SD |
17.4±3.8 |
17.1±2.8 |
^0.718 |
|
|
Surgery
type (N,
%) |
Hernia
repair |
17
(56.7%) |
19
(63.3%) |
§0.703 |
|
Hydrocele |
5
(16.7%) |
6
(20.0%) |
||
|
Orthopedic
in lower extremities |
5
(16.7%) |
2
(6.7%) |
||
|
Other
surgeries |
3
(10.0%) |
3
(10.0%) |
||
^Independent
t-test; #Chi square test; §Fisher's exact test.
Table 2: Surgical time, intraoperative motor block, and
anaesthetic value comparison.
|
Ketamine (N=30) |
Bupivacaine (N=30) |
P
value |
Ketamine's
impact in respect to bupivacaine |
||||
|
Mean±SD
|
95%
CI |
||||||
|
Operation
time (min), Mean±SD |
62.4±11.7 |
62.8±13.4 |
^0.894 |
-0.4±3.3 |
-6.9–6.1 |
||
|
|
|
|
|
RR |
95%
CI |
||
|
Bromage
scale |
0 |
24
(80.0%) |
16
(53.3%) |
§0.031* |
1.50 |
1.03–2.19 |
|
|
1 |
6
(20.0%) |
9
(30.0%) |
Reference |
||||
|
2 |
0
(0.0%) |
5
(16.7%) |
|||||
|
Anaesthesia
value |
Excellent |
16
(53.3%) |
7
(23.3%) |
#0.017* |
2.29 |
1.10–4.74 |
|
|
Good |
12
(40.0%) |
14
(46.7%) |
Reference |
||||
|
Moderate |
2
(6.7%) |
9
(30.0%) |
|||||
^Independent
t-test; §Fisher's Exact test; #Chi square test; *Significant; RR: Relative risk;
CI: Confidence interval.
Table 3: The means of heart rate, mean arterial pressure and
peripheral oxygen saturation at various times of measurements in the two
studied groups.
|
Time |
K/B (n=30) |
B/S (n=30) |
^P-value |
Effect
of ketamine relative to Bupivacaine |
||
|
Mean±SEM
|
95%
CI |
|||||
|
Heart rate (beat/minute) |
||||||
|
Baseline |
74.3±2.9 |
73.4±3.5 |
0.271 |
0.9±0.8 |
-0.7–2.6 |
|
|
IP, minute-5 |
81.1±2.7 |
76.0±3.6 |
<0.001* |
5.1±0.8 |
3.4–6.7 |
|
|
IP,
minute-10 |
89.2±2.3 |
80.7±3.1 |
<0.001* |
8.5±0.7 |
7.1–9.9 |
|
|
IP, minute-15 |
96.9±2.5 |
83.1±3.4 |
<0.001* |
13.7±0.8 |
12.2–15.3 |
|
|
IP,
minute-30 |
101.3±2.5 |
84.8±3.0 |
<0.001* |
16.5±0.7 |
15.1–17.9 |
|
|
IP, operation end |
105.5±3.4 |
85.7±4.1 |
<0.001* |
19.9±1.0 |
17.9–21.8 |
|
|
PO,
minute-5 |
106.1±2.9 |
86.9±3.3 |
<0.001* |
19.1±0.8 |
17.5–20.7 |
|
|
PO, minute-15 |
106.4±2.8 |
86.6±3.0 |
<0.001* |
19.8±0.8 |
18.3–21.3 |
|
|
PO,
minute-30 |
103.1±2.9 |
84.4±3.1 |
<0.001* |
18.7±0.8 |
17.1–20.3 |
|
|
Mean blood pressure (mmHg) |
||||||
|
Baseline |
71.9±3.2 |
71.3±2.5 |
0.447 |
0.6±0.7 |
-0.9–2.0 |
|
|
IP, minute-5 |
81.1±3.7 |
70.4±2.7 |
<0.001* |
10.8±0.8 |
9.1–12.4 |
|
|
IP,
minute-10 |
88.9±3.3 |
66.7±2.7 |
<0.001* |
22.2±0.8 |
20.6–23.8 |
|
|
IP, minute-15 |
95.3±3.3 |
66.8±2.7 |
<0.001* |
28.5±0.8 |
27.0–30.0 |
|
|
IP,
minute-30 |
99.5±3.6 |
65.7±3.3 |
<0.001* |
33.8±0.9 |
32.0–35.6 |
|
|
IP, operation end |
103.4±2.5 |
64.6±3.5 |
<0.001* |
38.8±0.8 |
37.3–50.4 |
|
|
PO,
minute-5 |
104.8±4.3 |
68.9±3.6 |
<0.001* |
36.0±1.0 |
33.9–38.0 |
|
|
PO, minute-15 |
103.4±3.0 |
71.4±2.9 |
<0.001* |
32.0±0.8 |
30.5–33.5 |
|
|
PO,
minute-30 |
102.8±4.3 |
75.5±3.6 |
<0.001* |
27.4±1.0 |
25.3–29.4 |
|
|
Oxygen saturation (%) |
||||||
|
Baseline |
99.5±0.5 |
99.6±0.5 |
0.447 |
-0.1±0.1 |
-0.4–0.2 |
|
|
IP, minute-5 |
99.0±0.6 |
99.1±0.6 |
0.521 |
-0.1±0.2 |
-0.4–0.2 |
|
|
IP,
minute-10 |
99.2±0.6 |
99.3±0.5 |
0.451 |
-0.1±0.1 |
-0.4–0.2 |
|
|
IP, minute-15 |
99.3±0.5 |
99.1±0.5 |
0.142 |
0.2±0.1 |
-0.1–0.5 |
|
|
IP,
minute-30 |
99.1±0.3 |
99.0±0.2 |
0.168 |
0.1±0.1 |
-0.1–0.2 |
|
|
IP, operation end |
99.0±0.5 |
99.0±0.6 |
0.999 |
0.0±0.1 |
-0.3–0.3 |
|
|
PO,
minute-5 |
99.3±0.6 |
99.3±0.7 |
0.999 |
0.0±0.2 |
-0.3–0.3 |
|
|
PO, minute-15 |
99.3±0.5 |
99.1±0.5 |
0.147 |
0.2±0.1 |
-0.1–0.5 |
|
|
PO,
minute-30 |
99.4±0.5 |
99.2±0.5 |
0.203 |
0.2±0.1 |
-0.1–0.4 |
|
Data
presented as Mean±SD; IP: Intraoperative; SE: Standard error; CI: Confidence
interval; ^Independent t-test; *Significant.
Table 4: Post-operative sedation score, period of micturition
and adjacent effects assessment.
|
Variables
|
Ketamine (N=30) |
Bupivacaine (N=30) |
t-test |
Outcome
of ketamine respect to Bupivacaine |
|
|
Mean±SD
|
95%
CI |
||||
|
Sedation
score, Mean±SD |
3.6±1.0 |
2.6±1.0 |
<0.001* |
-1.0±0.3 |
-1.5–-0.5 |
|
Time
to first micturition (hours), Mean±SD |
16.6±2.1 |
24.5±3.7 |
<0.001* |
-7.8±0.8 |
-9.4–-6.3 |
|
Time
to spontaneous eye opening (minutes), Mean±SD |
3.4±1.2 |
3.0±1.1 |
0.208 |
0.4±0.3 |
-0.2–0.9 |
|
|
|
|
|
RR |
95%
CI |
|
Nausea,
(n, %) |
2 (6.7%) |
7
(23.3%) |
§0.154 |
0.29 |
0.06-1.26 |
|
Vomiting,
(n, %) |
2
(6.6%) |
4
(13.3%) |
§0.512 |
0.34 |
0.05-4.04 |
|
Headache,
(n, %) |
4
(13.3%) |
8
(26.6%) |
#0.063 |
0.43 |
0.11-1.32 |
Table 5: Evaluation of parents' satisfaction with analgesia,
postoperative pain perception, and the need for analgesia.
|
Time
|
Ketamine (N=30) |
Bupivacaine (N=30) |
^ t-test |
Outcome
of ketamine respect to Bupivacaine |
|||
|
Mean±SD
|
Range
|
||||||
|
Post-operative
pain perception (VAS-10), Mean±SD |
|||||||
|
Minute-5 |
0.6±0.32 |
0.7±0.5 |
0.434 |
-0.1±0.11 |
-0.4–0.21 |
||
|
Minute-10 |
0.7±0.23 |
0.8±0.4 |
0.250 |
-0.1±0.11 |
-0.4–0.11 |
||
|
Minute-15 |
0.8±0.42 |
1.0±0.4 |
0.109 |
-0.2±0.1 |
-0.4–0.0 |
||
|
Minute-30 |
1.2±0.25 |
1.5±0.6 |
0.071 |
-0.3±0.1 |
-0.6–0.0 |
||
|
Minute-60 |
2.1±0.15 |
2.4±0.7 |
0.058 |
-0.3±0.2 |
-0.6–0.0 |
||
|
Minute-90 |
2.2±0.14 |
2.5±0.7 |
0.059 |
-0.3±0.21 |
-0.6–0.0 |
||
|
Minute-120 |
2.6±0.80 |
3.15±0.91 |
<0.01* |
-0.8±0.21 |
-1.2–-0.41 |
||
|
Minute-150 |
3.5±0.51 |
4.13±0.71 |
<0.01* |
-1.0±0.21 |
-1.3–-0.61 |
||
|
Minute-180 |
3.7±0.50 |
4.17±0.71 |
<0.01* |
-1.1±0.21 |
-1.5–-0.81 |
||
|
Analgesia
prerequisite, Mean±SD |
|||||||
|
Time
to first rescue analgesia (minutes) |
157.0±26.9 |
122.0±35.2 |
<0.001* |
35.0±8.1 |
18.8–51.2 |
||
|
Total
24-hours analgesia dose (gm) |
0.9±0.2 |
1.2±0.3 |
<0.001* |
-0.3±0.1 |
-0.5–-0.2 |
||
|
Parent’s
satisfaction, (n, %) |
|||||||
|
Grades |
|
|
|
RR |
95%
CI |
||
|
Fair |
2
(6.71%) |
17
(56.7%) |
#<0.001* |
0.12 |
0.03–0.47 |
||
|
Good |
7
(23.31%) |
8
(26.7%) |
Reference |
||||
|
Very
good |
10
(33.3%) |
4
(13.3%) |
|||||
|
Excellent |
11
(36.7%) |
1
(3.3%) |
|||||
^Independent
t-test; #Chi square test; *Significant; RR: Relative risk; CI: Confidence
interval.

IP: Intraoperative. PO: Postoperative. M: Minute. *Significant

IP: Intraoperative. PO: Postoperative. M: Minute. *Significant

IP: Intraoperative. PO: Postoperative. M: Minute. *Significant
IP: Intraoperative; PO: Postoperative; M: Minute; *Significant.

References
1. Pippal DK, Narang
N, Mukati R, Naveen RS (2020) Caudal Ketamine for Post-operative Analgesia in
Pediatric Lower Abdominal Surgeries. Int J Sci Study 8: 111-118.
2. Khan Q, Shua Nasir
Ba (2015) To Compare the Duration and side effects of Caudal Tramadol
Bupivacaine versus Ketamine–Bupivacaine for Postoperative analgesia in the
pediatric age group. Pakistan J Med Heal Sci 9: 1233-1236.
3. Farrag WSH, Ibrahim
AS, Mostafa MG, Kurkar A, Elderwy AA (2015) Ketamine versus magnesium sulfate
with caudal bupivacaine block in pediatric inguinoscrotal surgery: A
prospective randomized observer-blinded study. Urol Ann 7: 325-329. [Crossref]
4. Shirmohammadie M,
Soltani AE, Arbabi S, Nasseri K (2019) A randomized-controlled, double-blind
study to evaluate the efficacy of caudal midazolam, ketamine and neostigmine as
adjuvants to bupivacaine on postoperative analgesic in children undergoing
lower abdominal surgery. Acta Biomed 89: 513-518. [Crossref]
5. Naz U, Ilyas M,
Sifatullah A, Hassanain SS, Bangash R et al. (2020) Caudal block using Ketamine
with Bupivacaine and Bupivacaine alone for post-operative analgesia in
Paediatric inguino-scrotal surgeries. Pak J Surg 36: 90-95.
6. Gao M, Rejaei D,
Liu H (2016) Ketamine use in current clinical practice. Acta Pharmacol Sin
37: 865-872. [Crossref]
7. Dawson B, Trapp RG
(2004) Basic and clinical biostatistics. 2001: 141-142.
8. Wewers ME, Lowe NK
(1990) A critical review of visual analogue scales in the measurement of
clinical phenomena. Res Nurs Health 13: 227-236. [Crossref]
9. Bromage PR (1962)
Spread of analgesic solutions in the epidural space and their site of action: a
statistical study. Br J Anaesth 34: 161-178. [Crossref]
10. Sessler CN, Riker
RR, Ramsay MA (2013) Evaluating and monitoring sedation, arousal, and agitation
in the ICU. Semin Respir Crit Care Med 34: 169-178. [Crossref]
11. Khoshfetrat M,
Davoodi R, Keykha A (2018) Comparing the effects of three different doses of
caudal ketamine plus bupivacaine on pain control after paediatric surgery. Biomed
Res Ther 5: 2572-280.
12. Solanki NM,
Engineer SR, Jansari DB, Patel RJ (2016) Comparison of caudal tramadol versus
caudal fentanyl with bupivacaine for prolongation of postoperative analgesia in
pediatric patients. Saudi J Anaesth 10: 154-160. [Crossref]
13. Chandramohan D,
D’Souza SA (2016) Preservative-free racemic ketamine with bupivacaine: a
desirable option for extended caudal analgesia in pediatric surgery. Ain-Shams
J Anaesthesiol 9: 426-431.
14. Abd El AE-AA, Abd
Alla W (2015) Comparative study between caudal dexmedetomidine with bupivacaine
versus ketamine with bupivacaine for postoperative analgesia after
inguinoscrotal surgery in pediatric patients. Ain-Shams J Anaesthesiol
8: 634-638.
15. Amitha S, Metri V,
Mahadevaiah T, Yoganarasimha (2019) A Comparative Clinical Study between
Clonidine and Tramadol with Bupivacaine in Caudal Epidural for Postoperative
Analgesia in Pediatric Surgery. Anesth Essays Res 13: 389-394. [Crossref]
16. Shafqat E, Sameen Asghar,
Arshad Q, Ahmad S (2019) Caudal bupivacaine alone versus bupivacaine with
ketamine to compare postoperative analgesia. J Med Physiol Biophys 56:
1-8.
17. Kaur D, Anand S (2016) Comparison between caudal bupivacaine and bupivacaine with ketamine for postoperative analgesia in children: A prospective randomized clinical study. Anesth Essays Res 10: 488-492. [Crossref]
18. Ibraheem AS, Mohamed MA (2007) Caudal ketamine for pediatric postoperative analgesia: with or without bupivacaine. AAMJ 5: 186-200.
