Portal Vein Thrombosis as a Complication of Laparoscopic Sleeve Gastrectomy: A Case Report
A B S T R A C T
Portal vein thrombosis (PVT) is an uncommon and potentially life-threatening complication of bariatric surgery. Three cases of PVT were diagnosed at our regional center. All cases were post-laparoscopic sleeve gastrectomy without any intraoperative complications. All patients presented with vomiting and CT scans confirming PVT. No patients required operative management of venous mesenteric ischaemia and all were managed with anticoagulation. Two out of the three cases were found to have risk factors for venous thromboembolism. Surgeons should be aware of the vague symptomology of this rare entity and have a higher degree of suspicion in patients with risk factors of venous thrombosis.
Keywords
Bariatric surgery, portal vein thrombosis, sleeve gastrectomy
Introduction
Minimally invasive bariatric surgery has gained wide acceptance all over the world. Over the past 10 years, we have seen increasing numbers of such procedures being performed all over Australia, including rural centers. Laparoscopic sleeve gastrectomy is the most commonly performed operation [1]. With increasing exposure, advances in technology and training, complications related to bariatric surgery have continued to decline. Though despite advances in laparoscopic bariatric surgery, patients are still at significant risk of complications such as leaks, sepsis, bleeding and pulmonary embolus, especially considering the higher risk patient group. Portal vein thrombosis is a known complication of upper abdominal surgery but rarely reported in bariatric surgery and as such, diagnosis can be challenging.
Case Description
Case 1
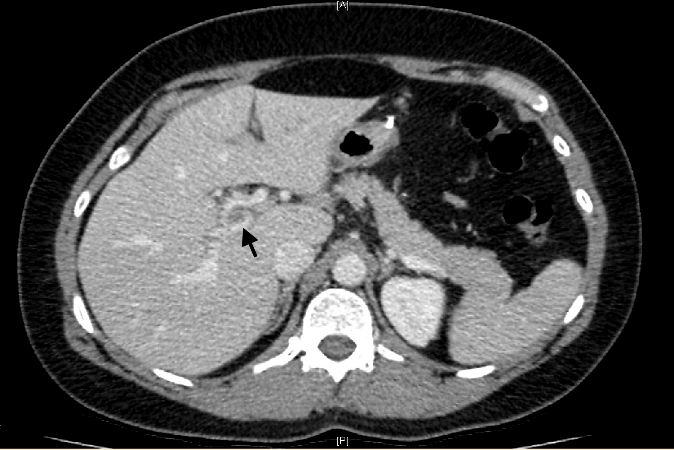
A 37-year-old female, with a history of smoking, on oral contraceptive pills, underwent a laparoscopic sleeve gastrectomy. She presented to the emergency department 11 days post-surgery with intractable vomiting not associated with any abdominal pain. Tachycardia was at 110 BPM, haemodynamically stable and afebrile. On examination, her abdominal exam finds a soft non-tender abdomen. Haematology demonstrated a WCC of 12.5 and a lactate of 1.8. A CT abdomen was performed and demonstrated extensive thrombosis of the intrahepatic portal vein branches, sparing the main portal, mesenteric and splenic vein (Figures 1 & 2). She was admitted and managed with supportive care, haematology specialist was consulted, and the patient was commenced on Warfarin. She was discharged home after 8 days of admission with warfarinisation for 6 months. Contraceptive pills were ceased. A hepatic portal vein ultrasound was performed 4 months post-treatment and demonstrated normal hepatopetal flow with no thrombosis and no evidence of portal hypertension.
Figure 1: CT Portal venous phase. Axial view. Thrombus in the portal vein.
Figure 2: CT Portal venous phase. Coronal view.
Case 2
A 45-year-old female with a history of smoking underwent a laparoscopic sleeve gastrectomy. She presented to the emergency department 10 days post-surgery with vomiting, epigastric abdominal pain and anorexia. She was haemodynamically stable, and her abdominal examination revealed a soft but tender epigastrium. Haematology demonstrated a WCC of 7.6 x10^9/L and a lactate of 1.5. A CT abdomen was performed and formally reported as normal, with no cause identified. The patient was admitted for supportive care. 2 days post-admission, a second radiology opinion was requested. Portal vein thrombosis was then reported with no evidence of bowel ischaemia. Furthermore, an ultrasound study of the portal venous system was performed confirming portal vein and splenic vein thrombosis.
A haematology specialist was consulted, and the patient was commenced on therapeutic anticoagulation Warfarin. A thrombophilia screen was performed, and the patient was discharged home 9 days post-presentation. On follow-up, the thrombophilia screen revealed a JAK2 V617F mutation. Subsequently a bone marrow biopsy was performed confirming an occult myeloproliferative disorder, the patient was continued on anticoagulation.
Case 3
A 53-year-old male underwent a laparoscopic sleeve gastrectomy. The patient presented to the emergency department 16 weeks post-surgery complaining of 4 days of abdominal discomfort, vomiting, anorexia and loose stools. On examination, the patient’s abdomen was found to be soft and mildly tender over the epigastrium. Haematology demonstrated a normal WCC of 8.2 x 10^9/L and a lactate of 1.8. A CT abdomen was performed that demonstrated portal vein thrombosis extending into the distal SMV and splenic vein with associated mesenteric oedema and a small amount of ascites. He was commenced on anticoagulation with Warfarin and discharged home in 5 days. At 4 months follow-up, a hepatic portal vein ultrasound was performed confirming resolution of thrombus and no evidence of portal hypertension.
Discussion
Portomesenteric vein thrombosis is most commonly associated with cirrhotic patients and patients with a prothrombotic disorder. Other causes include abdominal sepsis, pancreatitis and abdominal surgery [2]. Symptoms are vague abdominal pain and distension with nausea, vomiting and anorexia. Complications of PVT are acute intestinal ischaemia likely due to venous outflow obstruction and reflex arterial vasoconstriction [3]. Long-term complications are related to chronic PVT resulting in portal hypertension and in turn, ascites, varices, and portal cholangiopathy [3]. Retrospective studies have found PVT in 0.1-0.4% of laparoscopic bariatric surgery but this number may be an underestimate as silent PVT may as well be occurring [4]. Though a rare complication, it is associated with mesenteric ischaemia 5-15% of cases [5].
The exact cause of PVT in laparoscopic bariatric surgery is unknown but various mechanisms have been hypothesised based on principles of Virchow’s Triad of hypercoagulability, endothelial injury and stasis of blood flow [2, 4, 6, 7]. The most widely accepted opinion is the decreased splanchnic blood flow due to pneumoperitoneum achieved with pressures above 14mmhg, which has been shown in a study to decrease blood flow by up to 53% on ultrasound imaging [6]. Other factors include reverse Trendelenburg positioning causing iliac vessels and viscera compression, CO2 insufflation diffusing across peritoneum resulting in vasoconstriction, instrumentation resulting in damage to splanchnic vessels resulting in endothelial injury and thrombus formation, and a systemic hypercoagulability state in morbid obesity through various mechanisms such an elevated inflammatory state and endothelial dysfunction [2, 3].
Treatment of PVT is dependent on the extent of thrombosis and if evidence of intestinal ischaemia is present, which mandates urgent exploration to evaluate for ischaemic bowel [2]. The aim of the treatment is to recanalize the thrombosed vessel to prevent complications. The majority of cases can be managed with systemic anticoagulation, recommended for 6-12 months with heparin or vitamin K antagonists. Percutaneous trans-hepatic portal vein catheterization has been reported in the literature and can be used in more severe cases. Thrombophilia screening may be needed to investigate if any underlying prothrombotic conditions exist.
Conclusion
PVT is a rare complication of laparoscopic sleeve gastrectomy; its symptomology is variable and as such, can be a diagnostic dilemma. CT with portal venous phase is diagnostic for PVT but can be missed on reporting. Surgeons must have a higher index of suspicion in patients with risk factors of venous thromboembolism and involve haematology physicians early in the diagnosis. Operative intervention is seldom required however, close observation is necessary for the acute setting as venous mesenteric ischaemia can occur.
Article Info
Article Type
Case ReportPublication history
Received: Wed 02, Dec 2020Accepted: Wed 16, Dec 2020
Published: Mon 28, Dec 2020
Copyright
© 2023 Ramiz Iqbal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.02.11
Author Info
Corresponding Author
Ramiz IqbalDepartment of Surgery, John Hunter Hospital, Newcastle, New South Wales, Australia
Figures & Tables

References
- Campbell JA, Hensher M, Davies D, Green M, Hagan B et al. (2019) Long-Term Inpatient Hospital Utilisation and Costs (2007–2008 to 2015–2016) for Publicly Waitlisted Bariatric Surgery Patients in an Australian Public Hospital System Based on Australia’s Activity-Based Funding Model. Pharmacoecon Open 3: 599-618. [Crossref]
- Parikh S, Shah R, Kapoor P (2010) Portal vein thrombosis. Am J Med 123: 111-119. [Crossref]
- James AW, Rabl C, Westphalen AC, Fogarty PF, Posselt AM et al. (2009) Portomesenteric venous thrombosis after laparoscopic surgery: a systematic literature review. Arch Surg 144: 520-526. [Crossref]
- Goitein D, Matter I, Raziel A, Keidar A, Hazzan D et al. (2013) Portomesenteric thrombosis following laparoscopic bariatric surgery: incidence, patterns of clinical presentation, and etiology in a bariatric patient population. JAMA Surg 148: 340-346. [Crossref]
- Hmoud B, Singal AK, Kamath PS (2014) Mesenteric venous thrombosis. J Clin Exp Hepatol 4: 257-263. [Crossref]
- Jakimowicz J, Stultiens G, Smulders F (1998) Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc 12: 129-132. [Crossref]
- Trebicka J, Strassburg CP (2014) Etiology and Complications of Portal Vein Thrombosis. Viszeralmedizin 30: 375-380. [Crossref]
