Primary Vaginal Leiomyosarcoma: A Rare Case Reported in Uruguay
A B S T R A C T
Introduction: Primary vaginal sarcomas are very rare tumors and represent approximately 3% of vaginal cancers, and two-thirds are leiomyosarcomas. On this occasion we report the clinical case of a 35-year-old patient assisted by the Gynecology Oncology team of the Gynecology Clinic A, conducting a review of the bibliography to contribute to the management of this entity.
Clinical Case: 35-year-old patient with a diagnosis of primary high-grade vaginal leiomyosarcoma, presented with a vaginal mass, treatment was performed in two stages with tumorectomy and subsequently radical C1 hysterectomy, achieving complete resection of the mass, receiving radiation therapy, brachytherapy, and adjuvant chemotherapy. Thirty-one months after treatment, the patient is asymptomatic, with no elements of recurrence.
Conclusion: The treatment of these tumors is not well established. Complete surgical excision with wide resection margins is recommended. The use of radiotherapy and adjuvant chemotherapy must be individualized.
Keywords
Vaginal leiomyosarcoma, vaginal tumor, high-grade sarcoma
Introduction
Primary vaginal tumors are infrequent; in 2020, 17908 cases of vaginal cancer were reported worldwide according to data extracted from the WHO International Agency for Cancer Research [1]. The vagina is a common site of metastasis of tumors that originate in other organs or spread by direct extension, either from the female genital tract, such as the uterine cervix or endometrium, or from extragenital sites such as the rectum and bladder [2]. The most common type are carcinomas [3]. Primary vaginal sarcomas are very rare and correspond to approximately 3% of vaginal cancers, approximately two thirds of these are leiomyosarcomas [2, 4, 5]. Leiomyosarcomas generally develop in premenopausal women with a mean age of presentation of 53 years [6]. Their symptoms are nonspecific and may present with abdominopelvic pain and/or vaginal pain, or genitorrhagia. On physical examination, the tumors may appear as an elevated submucosal mass simulating a cyst. Some women have a history of pelvic radiation [6].
Due to its low incidence, gynaecologists are not familiar with it, causing a delay in its diagnosis, and treatment is not well standardized. This makes the interdisciplinary approach essential and includes pathologists, radiologists, surgeons, gynecologic oncologists, radiotherapists, and medical oncologists [2]. In this opportunity we present the case of a 35-year-old patient assisted by the Gynecologic Oncology team of the Gynecologic Oncology Clinic A of the School of Medicine of the University of the Republic with a diagnosis of primary leiomyosarcoma of the vagina, after obtaining informed consent, reviewing the literature to contribute to the treatment of this entity.
Clinical Case
We present a 35-year-old patient. No personal history of note.
I Obstetric and Gynaecological History
Menarche at 13 years of age. PAP SMEAR 2020: negative for malignancy. One previous pregnancy was a cesarean section in June 2020.
II History of Current Disease
During the third trimester of her pregnancy, in Mexico, a solid bleeding vaginal tumor was found. It presented with episodes of colporrhagia that determined hematologic repercussions. We have no other data regarding the physical examination at that time. The evaluation was complemented by magnetic resonance imaging (MRI) in December 2019, reporting a distended vaginal cavity at the expense of a bilobed lesion dependent on its right posterolateral wall that distends the vaginal fornix and compresses the rectum, measuring 91 × 70 × 60mm. Biopsies were taken in January 2020 and were inconclusive. The end of gestation was by cesarean section in June 2020. She lost contact with the health team during the puerperium, moving to Uruguay.
In July 2021, 13 months after birth, she contacted the medical team of the Pereira Rossell Hospital Center, where she consulted for the same symptoms, finding on physical examination a solid necrotic 7 cm tumor with apparent origin in the posterior lip of the uterine cervix, which presented itself as a degenerate myoma. A new magnetic resonance image was performed on 7/8/21 that reported a tumor in the vaginal cavity with imaging characteristics suggestive of cervical leiomyoma protruding into the vaginal cavity. A hysteroscopic lumpectomy was performed, finding in surgical exploration the presence of a bulky tumor that occupied the entire vagina, with necrotic areas, identifying its origin in the right and posterior vaginal fornix, with a macroscopic remanent tumor on the surgical site, not being able to complete removal in the first instance. Due to the diagnostic impression of invasion of the vaginal wall, a complementary diagnostic laparoscopy was performed and no alterations were identified in the pelvis. Pathological anatomy showed high-grade leiomyosarcoma, which was then referred to the Gynecologic Oncology Team of Gynecologic Clinic A, where she presented asymptomatic.
The evaluation was completed with an abdominal and pelvic magnetic resonance and chest tomography, shown in (Figure 1). In the abdomen and pelvis region, both ovaries had a normal appearance with multiple follicles and a functional laminar peri-ovarian liquid. Uterus in retroversion, with normal morphology. Vaginal parietal thickening in the upper third of the right lateral wall, with semiological elements suggesting a malignant nature related to the lesional remnant of high-grade leiomyosarcoma referred to in clinical data, measuring 43 × 33 × 51 mm in its longitudinal, transverse and anteroposterior diameters. No direct elements of parametrial involvement were identified. No elements suggesting regional or distant dissemination were identified. The complete surgical resection was decided in August 2021. A radical C1 hysterectomy was performed by laparotomy through an infraumbilical median incision.
Figure 1: Magnetic nuclear resonance of the abdomen and pelvis.
I) Axial section image of the pelvis from MRI. A) bladder, B) Vagina with gel, C) Sarcoma in the vagina. II) MRI sagittal section of pelvis image. A) Bladder, B) Vagina with gel, C) Sarcoma in vagina, D) Cervix, E) Uterine body.
Intraoperative findings include a normal sized uterus and a 5-cm tumor originating in the vagina involving the right paracolpos, the upper and middle third of the vagina. Intraoperative pathological analysis shows findings compatible with vaginal sarcoma with negative margins. A definitive pathological report shows 40 × 38 × 40 mm high-grade vaginal leiomyosarcoma located in the right lateral and posterior sectors. Microscopy shows 10 mitoses in 10 high magnification fields, ischemic necrosis areas, and no vascular embolisms. Free margins. No uterus or adnexal compromise (Figure 2).
Figure 2: Pathological anatomy images of high grade leiomyosarcoma.
A) Surgical specimen macroscopy observing atypical mesenchymal proliferation compatible with sarcoma. The tumor is seen on the right with a vaginal margin on the left, from which it is 2 mm away. B) H&E x10 staining of the surgical specimen where pleomorphic, spindle-shaped tumor cells with a pattern of nodules and fascicles, with an area of necrosis, are observed. C) Tumor cells are composed of heterochromatic nuclei with multiple mitoses. Staining with H&E x10. D) Proliferation of spindle cells with marked pleomorphism and mitotic count of 10 mitoses in 10 high-power fields. H&E stain x40. Images of the pathological anatomy report, courtesy of the Department of Pathological Anatomy and Cytology of the Women's Hospital, Dr. Paulina Luisi.
The patient received adjuvant chemotherapy, with 4 cycles based on Gemcitabine and Docetaxel, external pelvic radiotherapy, and brachytherapy in the vaginal vault. Thirty-six months after surgery she presented a good evolution, with no relapses.
Discussion
Vaginal leiomyosarcoma is the most common vaginal sarcoma; however, only 150 cases have been reported in the literature worldwide in the last 40 years, with presentation ages between 17 and 72 years [7]. About 50-60% of women with invasive vaginal cancer present with abnormal vaginal bleeding, frequently after sex, and may also present with vaginal discharge, palpable mass, dyspareunia, or pelvic or perineal pain [2]. In this case, the main symptom was a vaginal tumor, which was initially interpreted as a pedunculated fibroid protruding from the vagina; therefore, treatment was carried out in two stages, with oncological-directed treatment with definitive pathological anatomy results. The delay in the definitive diagnosis is reported in other studies such as the one carried out by the Mayo Clinic between 1908-1961, which reports 8 cases of primary leiomyosarcoma of the vagina [8]. Malkasian et al. reported predilection of the tumor for the posterior vaginal wall as in our case. This location contributes to the delay in treatment, since lesions can be incorrectly diagnosed as abscess, granuloma, rectocele, or cysts, generating a delay of 1 to 16 months in the definitive diagnosis [8].
The status of migrant in our case contributed to delays in definitive treatment, which led to the evaluation by two health teams with partial information from the patient's clinical history. The exact etiology of vaginal leiomyosarcomas is unknown, but exposure to pelvic radiotherapy and the insertion of vaginal implants have been implicated [9]. Our patient had none of these antecedents. These tumors can originate from any part of the vagina, but usually originate from the submucosa and smooth muscle of the vaginal wall. However, due to their anatomical proximity, they can arise from smooth muscle cells in any tissue adjacent to the vagina [10]. Malignancy depends on histological mitotic activity, cellular atypia, and necrosis [11]. In our case, corresponds to a T3N0M0 G2-3 tumor. There is no specific imaging method to evaluate these tumors; however, in MRI they generally appear as a heterogeneous, hyperintense mass, with irregular enhancement during the T1 phase after contrast administration [7].
Vaginal leiomyosarcomas spread through local invasion and hematogenous metastasis [12]. Despite the delay between the primary diagnosis of the vaginal tumor and the definitive treatment, our patient did not show distant or locoregional dissemination signs. Given their low incidence, there is no standard treatment for these tumors. Surgical resection is usually the main treatment. Peters et al. demonstrated a longer survival with wide resection, such as that provided by pelvic exenteration [10, 13]. Such aggressive treatment generates alterations in the quality of life in these patients, with repercussions on corporal imagen and sexuality, which is why it was not considered in our case. Kohsla et al. state that the primary treatment is complete resection with free margins, recommending resection margins of 1 to 2 cm, and 3 cm in high-grade tumors [7]. In our case, less than 1mm narrow margins were obtained.
In the event of positive or narrow margins, multimodal treatment of soft tissue sarcoma is required to avoid recurrences [2]. The National Comprehensive Cancer Network (NCCN) suggests that even after an entire macroscopic tumor resection (R0), adjuvant radiation therapy should be considered for high-risk metastasis tumors [14]. Routine lymphadenectomy is not indicated given the low incidence of lymph node metastasis [8].
Traditionally, postoperative radiotherapy has been used for the treatment of soft tissue sarcomas to reduce the incidence of local recurrence, while chemotherapy has a limited effect on treatment and no recommended pharmacological plan ([8, 12]. In this case, the patient was discussed in the institutional tumor committee and a multimodal approach was chosen, with surgery as primary treatment and radiotherapy, brachytherapy and adjuvant chemotherapy. The chemotherapy regimen used was aggressive, able to complete 4 cycles with gemcitabine and docetaxel, with no adverse severe effects during this treatment. Keller and Godoy reported the presence of adverse effects with this therapeutic plan, such as cellulitis and pancytopenia, the need for hospital admission, and the interruption of treatment due to them [15].
The main survival predictive factor is the degree of tumor differentiation and the clinical stage of the disease [7, 16]. Stage I has a 5-year survival rate of 55%; II, 44% and III and IV, 25% at 18 months. Age seems to influence prognosis, since patients under 40 years of age have a 5-year survival rate of 51%, while those over 50 years of age have a survival rate of 26% [6, 7, 16]. The pelvis is the first site of recurrence in all failed treatments [17]. Follow-up with physical examination and imaging is recommended every 3 to 6 months for two to three years then every 6 months for two years and then annually [14]. In the case of our patient, thirty-one months after treatment, she has not presented clinical or imaging elements of recurrence.
Conclusion
Primary vaginal leiomyosarcomas are aggressive low-frequency tumors. The recommended treatment is complete surgical excision, which has shown the best 5-year disease-free survival and overall survival rates. Adjuvant treatment with radiation therapy and/or adjuvant chemotherapy must be individualized.
Acknowledgements
The authors thank the Pathological Anatomy and Cytology team at the Women's Hospital, doctors Benedicta Caserta and Verónica Carbonatti, and Dr. Pablo Pedetti from the imaging service.
Author Contributions
Valeria Tolosa, Sebastian Ben, Diego Greif, Fernanda Nozar, Marcela Segredo, and Noelia Hernandez were direct participants in the patient's medical care. The literature review was directed by Valeria Tolosa, Marcela Segredo, and Noelia Hernandez. The analysis and writing of the first draft were done by Valeria Tolosa, Marcela Segredo, and Noelia Hernandez. Sebastian Ben, Diego Greif, and Fernanda Nozar revised the first draft of the manuscript. All authors revised the manuscript for the final version.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 25, Sep 2024Accepted: Thu 17, Oct 2024
Published: Tue 29, Oct 2024
Copyright
© 2023 Valeria Tolosa Villarreal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CROGR.2024.01.02
Author Info
Valeria Tolosa Villarreal Sebastián Ben Marcela Segredo Noelia Hernández Diego Greif Fernanda Nozar
Corresponding Author
Valeria Tolosa VillarrealGynecology and Obstetrics Clinic A, Pereira Rossell Hospital, School of Medicine, University of the Republic, Montevideo, Uruguay
Figures & Tables
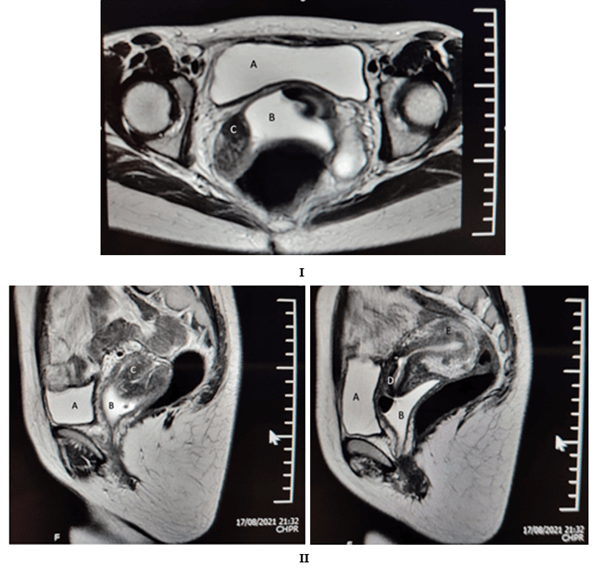
I) Axial section image of the pelvis from MRI. A) bladder, B) Vagina with gel, C) Sarcoma in the vagina. II) MRI sagittal section of pelvis image. A) Bladder, B) Vagina with gel, C) Sarcoma in vagina, D) Cervix, E) Uterine body.
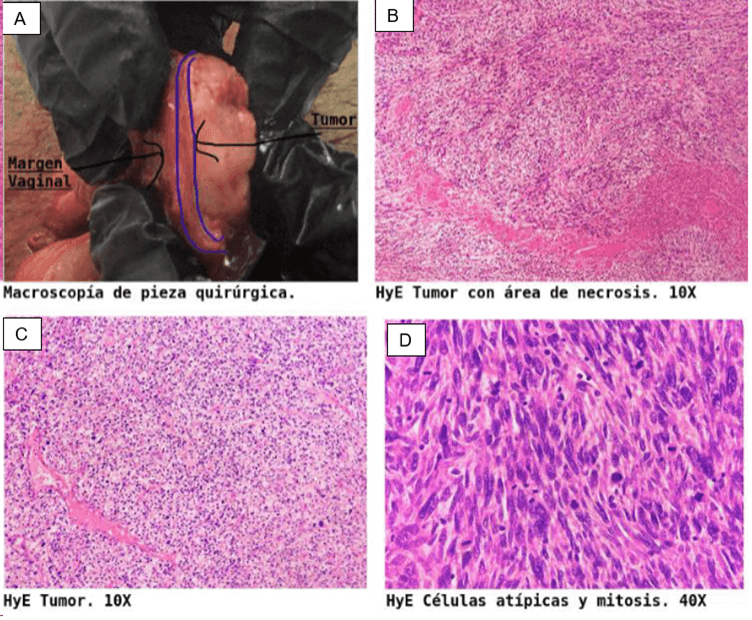
A) Surgical specimen macroscopy observing atypical mesenchymal proliferation compatible with sarcoma. The tumor is seen on the right with a vaginal margin on the left, from which it is 2 mm away. B) H&E x10 staining of the surgical specimen where pleomorphic, spindle-shaped tumor cells with a pattern of nodules and fascicles, with an area of necrosis, are observed. C) Tumor cells are composed of heterochromatic nuclei with multiple mitoses. Staining with H&E x10. D) Proliferation of spindle cells with marked pleomorphism and mitotic count of 10 mitoses in 10 high-power fields. H&E stain x40. Images of the pathological anatomy report, courtesy of the Department of Pathological Anatomy and Cytology of the Women's Hospital, Dr. Paulina Luisi.
References
1. WHO (2020) Cancer
Today, Global Cancer Observatory Estimated number of new cases in 2020, World
females all ages excl. NMSC.
2. Magné N, Pacaut C,
Auberdiac P, Jacquin J, Chargari C et al. (2011) Sarcoma of vulva, vagina and
ovary. Best Pract Res Clin Obstet Gynaecol 25: 797-801. [Crossref]
3.
Rastogi
BL, Bergman B, Angervall L (1984) Primary leiomyosarcoma of the vagina: a study
of five cases. Gynecol Oncol 18: 77-86. [Crossref]
4.
Wang
Y, Huang YW, Li YF (2015) Primary vaginal sarcoma: Experience of a regional
cancer center in China. J Obstet Gynaecol Res 41: 1463-1468. [Crossref]
5.
Fernández Romero C,
Rangel Y, Sutil Bayo S, Bordés Infantes M, Felipe Jimenez OD et al. (2018)
Leiomiosarcoma primario vaginal en el embarazo. A propósito de un caso. Revista Chilena de Obstetricia y Ginecología
83: 194-198.
6.
Devereaux
KA, Schoolmeester JK (2019) Smooth Muscle Tumors of the Female Genital Tract. Surg Pathol Clin 12: 397-455. [Crossref]
7.
Castaño Eguía MD,
Berdeal Fernández E, Alustiza Valdés JI, Garza Cantú A, García AJ (2022)
Leiomiosarcoma de vagina invasor a recto como causa de sepsis abdominal. Reporte
de un Caso 41: 42-46.
8. Malkasian Jr GD,
Welch JS, Soule EH (1963) Primary leiomyosarcoma of the vagina: Report of 8
cases. Am J Obstet Gynecol 86: 730-736. [Crossref]
9. Okunowo AA, Ugwu
AO, Owie E, Kolawole HF, Adebayo LA et al. (2020) Primary vaginal
leiomyosarcoma: Case report of a rare gynecological malignancy and Diagnostic
Challenge in a resource-constraint setting. Oxf Med Case Reports 2020:
omaa081. [Crossref]
10. Vizza E, Petrozza V, Porta N, Certelli C, Battaglione E et al. (2020) Primary vaginal
leiomyosarcoma: A case report with complete morphological, immunohistochemical
and ultrastructural study. Taiwan J Obstet Gynecol 59: 314-317. [Crossref]
11. Gong L, Liu H, Yang
K-X, Peng Z-L (2012) Stage IV primary vaginal leiomyosarcoma with lung and
breast metastases. Breast Care (Basel) 7: 150-152. [Crossref]
12. Behzatoğlu K,
Bahadir B, Inhan G, Altuğ M (2003) Primary vaginal leiomyosarcoma in pregnancy.
Gynecol Oncol 91: 627-629. [Crossref]
13. Peters WA, Kumar
NB, Andersen WA, Morley GW (1985) Primary sarcoma of the adult vagina: A
clinicopathologic study. Obstet Gynecol 65: 699-704. [Crossref]
14. Von Mehren M, Kane
JM, Agulnik M, Bui MM, Carr-Ascher J et al. (2022) Soft Tissue Sarcoma, Version
2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc
Netw 20: 815-833. [Crossref]
15. Ciaravino G, Kapp
DS, Vela AM, Fulton RS, Lum BL et al. (2000) Primary leiomyosarcoma of the
vagina. A case report and literature review. Int J Gynecol Cancer 10:
340-347. [Crossref]
16. Tsai HJ, Ruan CW, Kok VC, Li MC (2013) A large primary vaginal leiomyosarcoma diagnosed postoperatively and uterine leiomyomas treated with surgery and chemotherapy. J Obstet Gynaecol 33: 643-644. [Crossref]
