Psychological Problems Experienced by Primary Healthcare Workers During COVID-19 Epidemic in South Africa
A B S T R A C T
Background: The COVID-19 pandemic has negatively impacted on healthcare workers globally. The psychological impact of COVID-19 among primary healthcare workers who constitute a vulnerable group is yet to be evaluated in South Africa. The objectives were to estimate the prevalence and risk factors for stress, anxiety and depression among healthcare workers of a rural primary health care setting in South Africa.
Method: Self-administered questionnaire-based cross-sectional design was implemented among medical and nursing care professionals. Psychological problems were assessed using the Perceived Stress Scale (PSS-10), Generalized Anxiety Disorder (GAD-7) and Patient Health Questionnaire (PHQ-9). Logistic regression was performed to determine associated factors for psychological problems.
Results: The majority of HCWs were female (82.8%), of which 69.2% nurses and 56.6% single. The prevalence of stress, anxiety and depression disorders were 97.5%, 97.5% and 44% respectively. Females were 5.3 times (p<0.05) more likely to have stress disorder than males. Household size, perceived threat of family member not becoming infected with COVID-19 and having no concern of staff shortage were found to be protective for stress disorder (p<0.05). Healthcare workers who were not worried of getting infection and not worried of their family members getting infected found to be protective (OR<1, p<0.05) for anxiety disorder. Those 55 years or older were four times more likely to have depression (p<0.05) than their younger counterparts. Healthcare workers who were not worried of their family members would get infected and those were not worried to be infected were less likely (OR<1, p<0.05) to have depression disorder compared to those were worried.
Conclusion: Higher rates of stress, anxiety and depression were found among these HCWs. It is therefore imperative that appropriate and timely mental health care supports are provided to avert immediate and long term adverse psychological health outcomes of the HCWs.
Keywords
Anxiety, depression, stress, prevalence, perceived threat
Introduction
The global COVID-19 pandemic has led to unprecedented psychological problems more so to healthcare workers (HCWs) [1]. The HCWs all over the world including South Africa (SA) work under immense physical and psychological pressure. Although the earlier studies have described the outcomes of the disease being a mild form of infection, however, it is found that older adults and people with medical comorbidities are at higher risk of severe illness and death, with men at higher risk than women [2-4]. HCWs are at risk of exposure to highly infectious pathogens like COVID-19 generally while they care for patients or by exposure to patients environment or biological samples. The COVID-19 outbreak has impacted significantly on the HCWs and the general population of SA as there were 589,886 cases and 11,982 deaths as of 18 August 2020 [4]. During the same time the numbers of infected HCWs were 27,360; of which 78% were from the public and 22% from the private sectors with 240 deaths reported [4]. Thus such data must cause worry and concern to HCWs of becoming infected, possible death, and of transmission to family members. It is also important to note that besides infection, the social, demographic and economic problems that have resulted due to the COVID-19 pandemic is substantially and negatively affecting the psychosocial state of many individuals, including health care workers.
Healthcare workers in PHC facilities are facing tremendous pressure from the general population due to COVID-19. It has already been widely reported that panic of infection in the community, the high risk, often inadequate protection, loss of control, lack of experience in managing the disease, overwork, negative feedback from patients, perceived stigma, significant lifestyle changes, quarantine and lack of family support were attributed to psychological problems, associated with the pandemic [5-7]. On top of these problems, the provision of proper personal protective equipments (PPEs), training on the use and doffing off of all PPEs by HCWs are major concerns. These factors are likely to increase the incidence of psychological problems of HCWs especially at the lowest level of health facility in SA, such as fear, anxiety, depression, stress and insomnia, which are known to affect negatively on individual’s work efficiency and long-term well-being [8, 9]. Previous studies on HCWs exposed to similar infections such as the severe acute respiratory syndrome (SARS) outbreak in 2002-2003 found that psychological stress as a result of quarantine, reporting and monitoring of body temperature, and eventually refusal to patient care [10, 11]. The prevalence of symptoms of anxiety, depression, insomnia and the overall psychological problems in healthcare workers during the COVID-19 pandemic in China were 46%, 44%, 29% and 57% respectively [12].
It is reported that during the SARS 2003 epidemic in China that up to 35% of hospital healthcare workers suffered from a high-level of psychological distress and the symptoms of post-traumatic disorder that were higher than 10% after several years of the epidemic [4, 13]. The report further states that individuals who experienced quarantine or worked for in-patients with those infected were two to three times more likely to have post-traumatic stress disorders [13]. It is therefore recommended that a comprehensive understanding of the psychological problems experienced by healthcare workers during the COVID-19 epidemic are measured, with the aim of providing psychological support and assistance for the improvement of their mental health as HCWs are the key caregivers of the communities which they serve [14].
The WHO has also recommended that the countries of high COVID-19 infection take the necessary actions to address the negative impact of psychological health and well-being of HCWs including the general population [15]. However, there is no report available in SA that investigated psychological problems of HCWs are experiencing due to COVID-19. Therefore, the objectives of this study were to assess and estimate stress, anxiety and depression as psychological problems of COVID-19 among HCWs working at PHC setting in Durban, South Africa.
Methods
I Study Design
This was a cross-sectional study conducted among medical, allied and nursing care professionals at a Primary Health Care (PHC) facility in Durban, South Africa. The study settings, subjects and participant selection strategy was explained elsewhere [16].
II Questionnaire, Data collection and Measurements
Data were collected using a self-administered anonymous questionnaire. The questionnaire was developed by the researchers using different published articles [12, 17, 18]. The questionnaire dealt with HCWs demographics, personal, household (HH) risk factors and psychological symptoms related to stress, anxiety and depression. The questionnaire dealt with HCWs demographics: age, gender, category of health care worker, marital status and household size. Information regarding perceived threats and concerns of HCWs on the COVID-19 epidemic were also collected. Perceived Stress Scale (PSS-10) was used (considered as a classic stress assessment instrument) to measure perceived stress of HCWs [17]. Anxiety questions from Generalized Anxiety Disorder (GAD-7) and Patient Health Questionnaire scales (PHQ-9) were adapted to measure anxiety and depression [19, 20]. Seven-Items for GAD-7 and nine-items for PHQ-9 symptom questions were used respectively to measure anxiety and depression problems during the past 2 weeks [12].
III Data Analysis
Data were captured in Microsoft excel, coded, and transported and analysed using SPSS version 22.0. Descriptive statistics were used such as mean with standard deviation (SD) for continuous variables and frequency distribution for categorical variables. The prevalence of symptoms of stress, anxiety and depression were reported. The PSS-10 score ranged from 0 to 40 with higher scores indicating higher perceived stress. Scores ranged from 0 to 13 were considered low, from 14 to 26 moderate and from 27 to 40 considered high perceived stress respectively.
Both anxiety and depression problems were measured using cutoff points of the total scores 5, 10 and 15 to classify or categorise as mild, moderate and severe anxiety and depression respectively based on previous recommendation [21]. Therefore, total scores for GAD-7 and PHQ-9 were seperately categorized to represent: (1-5) none or minimal, (6-9) mild, (10-14) moderate and (> 15) severe anxiety and depression. However, the cut off points of PSS-10 scores > 14 for stress disorder, GAD-7 and PHQ-9 scores > 10 for anxiety and depression disorders were considered based on previous published studies [21, 22]. Pearson’s correlation test was conducted to determine the relationship between stress, anxiety and depression scores and reported results only those of p<0.05. The PSS-10 (scores > 14 = 1 and <13=0), GAD-7 (score > 10 =1 and < 9=0) and PHQ-9 (scores >10=1 and < 9=0) were treated as dichotomous variables for the univariate and bivariate analysis. Cross table analysis using the chi-square test and p values were reported to identify whether variables had significant difference of prevalence of stress, anxiety and depression with demographic and other variables. The variables that had significant association were used in Binary logistic regression (backward) analysis to determine significant predictors for stress, anxiety and depression disorders. The results reported OR (adjusted odds ratio) with 95% Confidence Interval (CI). All tests were two-tailed, with a significance level of p<0.05.
Results
A total of 159 HCWs completed the self-administered questionnaire resulting a response rate of 87%. Table 1 depicted the demographic and risk profile of the HCWs. Female (82.8%) and nursing professionals constituted the majority (69.2%) among the HCWs. Nearly two-thirds (63.5%) of them were between the ages of 20 to 44 years, while 44% were single. The mean number of people living in a HH was 4.2 (SD=1.3) and 66% HH had between one and four people. About half (47.8%) of them used to undertake regular exercise before the pandemic but the percentage significantly dropped to 28.3% during the pandemic.
Table 1: Demographic and risk profile of the healthcare workers.
|
Variables |
Frequency |
Percentage |
|
Gender (n=157) |
|
|
|
Male |
27 |
17.2 |
|
Female |
130 |
82.8 |
|
Marital status (n=158) |
|
|
|
Single |
70 |
44 |
|
Married |
67 |
42.1 |
|
Other |
21 |
13.2 |
|
Age (n=159) |
|
|
|
20-34 years |
49 |
30.8 |
|
35-44 years |
52 |
32.7 |
|
45-54 years |
37 |
23.3 |
|
=> 55 years |
19 |
11.9 |
|
Category of staff (n=159) |
|
|
|
Nursing professional |
110 |
69.2 |
|
Medical and allied professionals |
49 |
30.8 |
|
Household size (n=145) |
|
|
|
1- 4 people per house |
105 |
66.0 |
|
> 5 people per house |
44 |
34 |
|
Mean no of people per HH (SD) |
4.26 (1.89) |
|
|
Exercise before COVID-19 pandemic |
76 |
47.8 |
|
Exercise during COVID-19 pandemic |
45 |
28.3 |
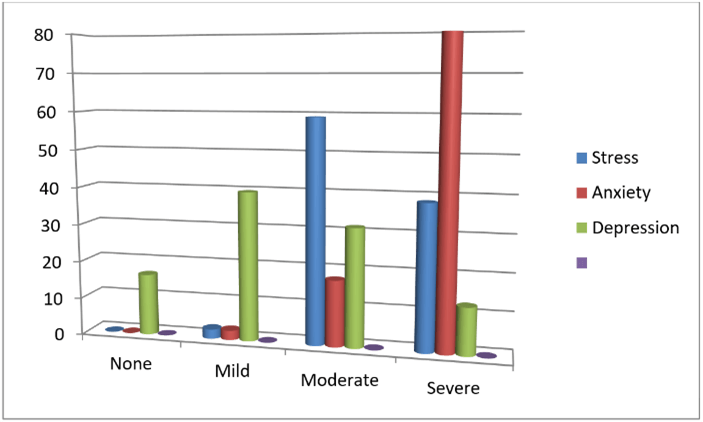
Figure 1: Frequency distribution of stress, anxiety and depression of HCWs.
The HCWs of this PHC facility showed a high-level perceived threat and concern for the COVID-19 epidemic (Table 2). All were concerned about adequate PPEs supply, while 96% were troubled about the public response to the epidemic. Other major concerns were that they (HCW) were worried of getting infection (91%), and someone in the workplace may get infected with the virus (94%).
Table 2: Perceived threats and concerns of healthcare workers related to COVID-19 epidemic.
|
Variables |
Frequency |
Percentage |
|
Worried to be infected by COVID-19 (n=159) |
120 |
75.5 |
|
Worried that family members will get infected by COVID-19 (n=159) |
99 |
62.3 |
|
Concern about becoming infected with COVID-19 (n=159) |
145 |
91.2 |
|
Concern that someone in the workplace will get infected with COVID-19 (n=159) |
150 |
94.3 |
|
Concern that someone in the personal network will get severely ill from COVID-19 (n=159) |
146 |
91.8 |
|
Concern that the health facility will not have enough PPE supplies to handle the COVID-19 outbreak (yes) (n=159) |
159 |
100. |
|
Concern of public response to COVID -19 epidemic (not good) |
149 |
96.1 |
|
Concern of staff shortage (n=158) |
18 |
11.4 |
All participating HCWs had some level of stress during the COVID-19 pandemic. More than half of the HCWs (59.1%) reported moderate levels while 38.4% had reported severe stress (Figure 1). Most of the HCWs (80%) reported severe anxiety and 17.6% moderate anxiety (Figure 1). The prevalence of mild to moderate depression symptoms were reported by 71% healthcare workers. Severe depression symptoms were found among 12.6% HCWs. Considering the generalized stress, anxiety and depression disorder among HCWs (PSS-10 scores > 14, GAD-7 and PHQ-9 scores >10 individually) 97.5%, 97.5% and 44% HCWs were recorded with stress, anxiety and depression disorders respectively.
Table 3: Pearson Correlations test results of stress, anxiety and depression scores or problem.
|
|
Total stress |
Total anxiety |
Total Depression |
|
|
Total PSS |
Pearson Correlation |
1 |
.394** |
.126 |
|
Sig. (2-tailed) |
|
.000 |
.113 |
|
|
N |
159 |
159 |
159 |
|
|
Total anxiety |
Pearson Correlation |
.394** |
1 |
.239** |
|
Sig. (2-tailed) |
.000 |
|
.002 |
|
|
N |
159 |
159 |
159 |
|
|
Total Dep |
Pearson Correlation |
.126 |
.239** |
1 |
|
Sig. (2-tailed) |
.113 |
.002 |
|
|
|
N |
159 |
159 |
159 |
|
**: Correlation is significant at the 0.01 level (2-tailed).
Pearson correlation test (Table 3) showed that stress scores were significantly positively correlated with anxiety scores (r=0.394; p<0.05). Anxiety scores were positively correlated with depression scores (r=.239; p<0.05).
Binary logistic regression analysis was therefore performed to identify demographic, perceived threat and concerns indicators which were associated with stress (PSS-10 score > 14), anxiety (GAD-7 score >10) and depression (PHQ-9 score >10) (Tables 4-6).
Table 4: Multiple logistic regression output for stress disorder.
|
Variables |
Sig. |
Exp(B) |
95% C.I. for EXP(B) |
|
|
Lower |
Upper |
|||
|
Gender (Female) |
.011 |
5.346 |
1.465 |
19.505 |
|
Gender (Male) |
.094 |
2.524 |
.855 |
7.448 |
|
Age < 34 years |
.124 |
|
|
|
|
Age 35-44 years |
.143 |
.339 |
.080 |
|
|
Age 45-54 years |
.512 |
1.515 |
.438 |
3.832 |
|
Age > 55 years |
.762 |
1.229 |
.323 |
.999 |
|
HH size 1-4 people |
.045 |
.386 |
.152 |
.978 |
|
Do think anyone in personal network will get COVID-19 (1) |
.084 |
.157 |
.019 |
1.287 |
|
Not worried that family members will get infected by COVID-19 (1) |
.050 |
.469 |
.221 |
.999 |
|
Not worried that anyone in personal network will get COVID-19 (1) |
.084 |
.157 |
.019 |
1.287 |
|
Concern of staff shortage |
.014 |
|
|
|
|
Shortage of staff (Yes) |
.173 |
.367 |
.087 |
1.553 |
|
Shortage of staff (No) |
.005 |
.267 |
.107 |
.668 |
|
Constant |
.583 |
.585 |
|
|
Female HCWs were 5.3 times (OR=5.3, p =0.011) more likely to have stress disorder than their male counterpart. Household size less than four was 62% less likely to have stress than HH with > 5 people (OR=0.38, p=0.045). Respondents who were not worried that family members will get infected by COVID-19 was 54% less likely to have stress disorder (OR=0.46, p=0.05). Having no concern of staff shortage was 74% less likely to have stress disorder (OR=.267, p=0.005). No demographic variable was associated with anxiety disorder. However, HCWs who were not worried of getting infected by COVID-19, 93% less likely to have anxiety (OR=0.072, p=0.046). Similarly, HCWs who were not worried of family members getting infected 98% less likely to have anxiety disorder (OR=0.02, p=0.003).
Table 5: Logistic regression output for anxiety disorder.
|
Variables |
Sig. |
Exp (B) |
95% C.I.for EXP (B) |
|
|
Lower |
Upper |
|||
|
Not worried of getting infected by COVID-19 (1) |
.046 |
.072 |
.006 |
.952 |
|
Not worried of family members get infected with COVID-19 (1) |
.003 |
.021 |
.002 |
.273 |
|
Constant |
.000 |
533.678 |
|
|
HCWs who were 55 years or older were four times more likely to have depression disorder (OR=4.1, p=0.029) than the younger HCWs. HCWs who did not think that their family members will get infected by COVID-19 were 55% less likely to have depression disorder (OR=0.45, p=0.033). HCWs those were not worried to be infected with COVID-19 were 90% less likely to have depression disorder (OR=0.10, p=0.032).
Table 6: Multiple logistic regression output for depression disorder.
|
Variables |
Sig. |
Exp (B) |
95% C.I. for EXP (B) |
|
|
Lower |
Upper |
|||
|
Category age |
.277 |
|
|
|
|
Age < 34 years |
.999 |
605.69 |
.000 |
. |
|
Age 35-44 years |
.120 |
2.67 |
.773 |
9.286 |
|
Age 45-54 years |
.056 |
3.33 |
.972 |
11.431 |
|
Age > 55 years |
.029 |
4.19 |
1.162 |
15.111 |
|
Were not worried of family members getting infected by (0) |
.033 |
.452 |
.218 |
.937 |
|
Were not worried of getting infected (0) |
.032 |
.103 |
.013 |
.822 |
|
Constant |
.011 |
.200 |
|
|
Discussion
This study provides an initial insight of the psychological problems of HCWs from PHC facilities during the COVID-19 epidemic in SA. This study is unique because it is the first study to describe the prevalence of stress, anxiety and depression due to the COVID-19 pandemic. The study followed an appropriate method of collecting and reporting information from all healthcare workers of PHC facilities. Most of the published reports on psychological problems of healthcare workers or general population were on voluntary basis and web-based thus had selection bias and lack generalizability.
The demographic indicators of HCWs indicated that majority were female (83%) of which 69% were nursing professionals. Their age group was < 45 years (63%), as younger professionals need to gain experience on the first level of healthcare services before they move or are promoted to higher levels. The mean HH size within this group was reasonable and was regarded as protective for stress disorder. Overall, there was a 41% reduction in good practice of regular exercise. This could be the result of national complete lockdown during the epidemic when the gyms were closed and walking or running in public places were banned.
The prevalence of stress, anxiety and depression were similar among all categories of staff (medical and nursing). All of whom reported mild to severe form of stress. There were no significant difference of prevalence of stress, anxiety and depression among these different professionals. It is so because of their level of health facility and type of care they provide together as a team. Notably 97.5% were categorized as stress disorder. This rate was higher than the rates reported from general population and HCWs from Saudi Arabia and China [23, 24]. Meta-analysis of five separate studies estimated stress among general population between 24.3% to 35.4% [23]. A lower rate of stress (41%) than the rate of our study was reported from Saudi Arabia among tertiary hospital HCWs before the incidence of any case of COVID-19 [24]. None of the other reported studies had estimated stress disorder in PHC workers. The higher level of stress among these PHC healthcare workers were likely as they were facing tremendous pressure from the general population due to the COVID-19 pandemic in SA and as they were dealing with suspected or confirmed cases of COVID-19 from the community and fellow co-workers. Literature has shown that healthcare workers are stressful about either being infected or infecting others in their household when providing medical care during an infectious outbreak [25]. Female HCWs were found with higher risk of stress in this setting. Females were known to be more prone to develop mental health problems and might had a higher workload and greater risk of direct exposure to patients with COVID-19 [25].
I Anxiety
There was a higher prevalence of anxiety disorder (97.5%). Among them, 18% moderate and a higher rate of 80% reported severe anxiety symptoms/disorders. This rate was considered higher compared to the findings from China and Saudi Arabia where they found 46% and 29% respectively among HCWs and between 24%-35% among general population [12, 23, 24]. The highest prevalence of anxiety disorder was observed in public health professionals in China (62.40%) [12]. The highest rate of anxiety among the PHC healthcare workers might be related to higher risk of infection and on account of being directly exposed to patients with COVID-19 with their contacts, perceived threats and concerns expressed by the HCWs together with tedious work involved in caring of positive cases.
The majority (71%) healthcare workers had mild to moderate depression symptoms. Severe depression symptoms (PHQ-9 score > 15) were found among 12.6% HCWs. The prevalence of depression disorder was 44% (31.4% moderate and 12.6% severe depression). This rate is similar to the findings of other studies from China that 44% were found with depression disorder and elsewhere [12, 26]. Identified risk facor for depression disoder was among older age (> 55 years) are similar to other study results from China [27]. Using a risk stratification tool for identification of psychological problems of HCWs in England age was a significant predictors, for example; mortality from COVID-19 was doubled among 50-59 years, quadrupled among 60-69 years and 12 times higher after the age of 70 years age groups [19]. The National Institute for Occupational Health in South Africa reported that, the median age of COVID-19 HCW admissions in SA was 44 years, 10% admissions among 60 years and older and majority (80.7%) being female [28]. The protective factors were HCWs perceived threats and concerns; who were not worried of their family members will get infected and those were not worried to be infected with COVID-19. This is true as these factors can put individuals at mental ease.
The results of this study was interesting as because those having perceived threats and concerns regarding the COVID-19 epidemic were associated with a higher risk of psychological problems (stress, anxiety and depression). Moreover, the infectious nature of COVID-19 and as a preventive measure, HCWs may be separated from their families to reduce the risk of transmission within families and communities. Research had shown that worrying about family members was one of the main sources of stress among nurses and medical doctors, indicating the critical need of support for PHC workers mental health [29, 30]. Similar to nurses, physicians are also under great stress, and nearly half of the physicians reported anxiety and depression. However, majority of the physicians were male and may have a higher acceptance of risk than nurses and have better coping skills [31].
II Factors Influencing Psychological Status of HCWs
The reported findings of the same healthcare workers were found with poor knowledge and poor preventive practices of COVID-19 epidemic and also found with higher prevalence of stress, anxiety and depression as psychological disorders [16]. Previous studies reported that good knowledge on cardiac disease led to improved quality of life and reduced psychological problems such as stress, anxiety and depression and this could be true that due to poor knowledge of HCWs resulted in reporting such higher prevalence of stress, anxiety and depression among these HCWs [32]. As the HCWs from other reports were showing nervous and panic of infection, perception of inadequate protection, lack of experience, lack of support in managing the disease, often overworked, experienced staff shortage, received negative feedback from patients all played negatively on them [5-7]. This ultimately reminded us of the importance of providing necessary psychological support to healthcare workers would require during the pandemic. Healthcare workers’ knowledge and skills need to be improved so that they are well equipped to cope with infectious disease and steps should be taken to provide necessary support to reduce the risk of infection and improve the working environment [31].
Conclusion
High rate of negative psychological symptoms were evident among healthcare workers during the COVID-19 pandemic in this study. It is of great importance to screen, manage and provide timeous psychological support for healthcare workers with adverse mental or psychological problems, who are at the frontline in providing care for patients infected with COVID-19 attending PHC facilities. Due to the profound and negative consequences of psychological impairment in these frontline workers, policymakers should also consider long term preventive measures to alleviate the development of adverse psychological symptoms.
Strengths and Limitation
The strength of this study is that it is the first study that evaluated the mental health of primary level health care workers to establish the prevalence of psychological or mental health problems that might have resulted due to the COVID-19 epidemic in SA. Despite these strengths, this study has some possible weaknesses. The small sample size might have caused the findings to be underpowered. Thus, the causal relationships should be interpreted with caution. The inherent limitation of cross-sectional study is unable to account for potential changes in psychological disorders over a longer period of time. More studies are needed to explore the longitudinal trajectories of stress, anxiety and depression disorders in healthcare workers of PHC settings during the COVID-19 pandemic and thereafter in SA. Moreover, the number of medical officers and allied health workers who participated in this survey was limited, that limited the generalizability of our results. The findings were based on self-reported questionnaires that investigated psychological problems, which might be different from clinical diagnostic interviews.
Ethical Consideration
Ethical approval was obtained from Umgungundlovu Health Ethics Research Board (Reference no. UHERB 007/2020). Permission from the KCHC management was obtained to undertake the study. Anonymity and confidentiality of the respondent was maintained at all times. Participation in the study was voluntary. The study obtained informed consent from the participants after explaining the purpose, nature and objectives of the study.
Acknowledgement
We thank all the participants who voluntarily took part in this study.
Competing Interests
None.
Conflicts of Interest
None.
Author Contributions
AMH, MEH: Conceptualisation, analysis, writing and finalization of the manuscript; SB, MH: Data collation, analysis and finalization of the manuscript; NS, AMA: Conceptualisation and finalization of the manuscript.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 30, Dec 2020Accepted: Mon 11, Jan 2021
Published: Fri 19, Feb 2021
Copyright
© 2023 Akm Monjurul Hoque. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.PDR.2021.01.01
Author Info
Akm Monjurul Hoque Somaya Buckus Maariyah Hoque ABM Mahbub ul Alam ME Hoque N Singh
Corresponding Author
Akm Monjurul HoqueKwadabeka Community Health Centre, Kwadabeka, South Africa
Figures & Tables
Table 1: Demographic and risk profile of the healthcare workers.
|
Variables |
Frequency |
Percentage |
|
Gender (n=157) |
|
|
|
Male |
27 |
17.2 |
|
Female |
130 |
82.8 |
|
Marital status (n=158) |
|
|
|
Single |
70 |
44 |
|
Married |
67 |
42.1 |
|
Other |
21 |
13.2 |
|
Age (n=159) |
|
|
|
20-34 years |
49 |
30.8 |
|
35-44 years |
52 |
32.7 |
|
45-54 years |
37 |
23.3 |
|
=> 55 years |
19 |
11.9 |
|
Category of staff (n=159) |
|
|
|
Nursing professional |
110 |
69.2 |
|
Medical and allied professionals |
49 |
30.8 |
|
Household size (n=145) |
|
|
|
1- 4 people per house |
105 |
66.0 |
|
> 5 people per house |
44 |
34 |
|
Mean no of people per HH (SD) |
4.26 (1.89) |
|
|
Exercise before COVID-19 pandemic |
76 |
47.8 |
|
Exercise during COVID-19 pandemic |
45 |
28.3 |
Table 2: Perceived threats and concerns of healthcare workers related to COVID-19 epidemic.
|
Variables |
Frequency |
Percentage |
|
Worried to be infected by COVID-19 (n=159) |
120 |
75.5 |
|
Worried that family members will get infected by COVID-19 (n=159) |
99 |
62.3 |
|
Concern about becoming infected with COVID-19 (n=159) |
145 |
91.2 |
|
Concern that someone in the workplace will get infected with COVID-19 (n=159) |
150 |
94.3 |
|
Concern that someone in the personal network will get severely ill from COVID-19 (n=159) |
146 |
91.8 |
|
Concern that the health facility will not have enough PPE supplies to handle the COVID-19 outbreak (yes) (n=159) |
159 |
100. |
|
Concern of public response to COVID -19 epidemic (not good) |
149 |
96.1 |
|
Concern of staff shortage (n=158) |
18 |
11.4 |
Table 3: Pearson Correlations test results of stress, anxiety and depression scores or problem.
|
|
Total stress |
Total anxiety |
Total Depression |
|
|
Total PSS |
Pearson Correlation |
1 |
.394** |
.126 |
|
Sig. (2-tailed) |
|
.000 |
.113 |
|
|
N |
159 |
159 |
159 |
|
|
Total anxiety |
Pearson Correlation |
.394** |
1 |
.239** |
|
Sig. (2-tailed) |
.000 |
|
.002 |
|
|
N |
159 |
159 |
159 |
|
|
Total Dep |
Pearson Correlation |
.126 |
.239** |
1 |
|
Sig. (2-tailed) |
.113 |
.002 |
|
|
|
N |
159 |
159 |
159 |
|
**: Correlation is significant at the 0.01 level (2-tailed).
Table 4: Multiple logistic regression output for stress disorder.
|
Variables |
Sig. |
Exp(B) |
95% C.I. for EXP(B) |
|
|
Lower |
Upper |
|||
|
Gender (Female) |
.011 |
5.346 |
1.465 |
19.505 |
|
Gender (Male) |
.094 |
2.524 |
.855 |
7.448 |
|
Age < 34 years |
.124 |
|
|
|
|
Age 35-44 years |
.143 |
.339 |
.080 |
|
|
Age 45-54 years |
.512 |
1.515 |
.438 |
3.832 |
|
Age > 55 years |
.762 |
1.229 |
.323 |
.999 |
|
HH size 1-4 people |
.045 |
.386 |
.152 |
.978 |
|
Do think anyone in personal network will get COVID-19 (1) |
.084 |
.157 |
.019 |
1.287 |
|
Not worried that family members will get infected by COVID-19 (1) |
.050 |
.469 |
.221 |
.999 |
|
Not worried that anyone in personal network will get COVID-19 (1) |
.084 |
.157 |
.019 |
1.287 |
|
Concern of staff shortage |
.014 |
|
|
|
|
Shortage of staff (Yes) |
.173 |
.367 |
.087 |
1.553 |
|
Shortage of staff (No) |
.005 |
.267 |
.107 |
.668 |
|
Constant |
.583 |
.585 |
|
|
Table 5: Logistic regression output for anxiety disorder.
|
Variables |
Sig. |
Exp (B) |
95% C.I.for EXP (B) |
|
|
Lower |
Upper |
|||
|
Not worried of getting infected by COVID-19 (1) |
.046 |
.072 |
.006 |
.952 |
|
Not worried of family members get infected with COVID-19 (1) |
.003 |
.021 |
.002 |
.273 |
|
Constant |
.000 |
533.678 |
|
|
Table 6: Multiple logistic regression output for depression disorder.
|
Variables |
Sig. |
Exp (B) |
95% C.I. for EXP (B) |
|
|
Lower |
Upper |
|||
|
Category age |
.277 |
|
|
|
|
Age < 34 years |
.999 |
605.69 |
.000 |
. |
|
Age 35-44 years |
.120 |
2.67 |
.773 |
9.286 |
|
Age 45-54 years |
.056 |
3.33 |
.972 |
11.431 |
|
Age > 55 years |
.029 |
4.19 |
1.162 |
15.111 |
|
Were not worried of family members getting infected by (0) |
.033 |
.452 |
.218 |
.937 |
|
Were not worried of getting infected (0) |
.032 |
.103 |
.013 |
.822 |
|
Constant |
.011 |
.200 |
|
|
References
- Zhu N, Zhang D, Wang W, Li X, Yang B et al. (2020) A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med 382: 727-733. [Crossref]
- Zhou F, Yu T, Du R, Fan G, Liu Y et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054-1062. [Crossref]
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323: 1239-1242. [Crossref]
- Onder G, Rezza G, Brusaferro S (2020) Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA 323: 1775-1776. [Crossref]
- Kang L, Li Y, Hu S, Chen M, Yang C et al. (2020) The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 7: e14. [Crossref]
- Chong MY, Wang WC, Hsieh WC, Lee CY, Chiu NM et al. (2004) Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry 185: 127-133. [Crossref]
- Maunder R (2004) The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci 359: 1117-1125. [Crossref]
- Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B et al. (2006) Longterm psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis 12: 1924-1932. [Crossref]
- McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KWT et al. (2007) Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 52: 241-247. [Crossref]
- Chan AO, Huak CY (2004) Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond) 54: 190-196. [Crossref]
- Brug J, Aro AR, Oenema A, de Zwart O, Richardus JH et al. (2004) SARS risk perception, knowledge, precautions, and information sources, the Netherlands. Emerg Infect Dis 10: 1486-1489. [Crossref]
- Que J, Shi L, Deng J, Liu J, Zhang L et al. (2020) Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 33: e100259. [Crossref]
- Wu P, Fang Y, Guan Z, Fan B, Kong J et al. (2009) The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 54: 302-311. [Crossref]
- Bao Y, Sun Y, Meng S, Shi J, Lu L (2020) 2019-nCoV epidemic: address mental health care to empower society. Lancet 395: e37-e38. [Crossref]
- Yao H, Chen JH, Xu YF (2020) Rethinking online mental health services in China during the COVID-19 epidemic. Asian J Psychiatr 50: 102015. [Crossref]
- Hoque AM, Bukus S, Hoque M, Hoque ME (2020) Knowledge, Attitude & Practices of Primary Healthcare Workers on COVID-19 from a Rural Setting of KwaZulu-Natal, South Africa. Clin Experiment Investig.
- Cohen S, Kamarch T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24: 385-396. [Crossref]
- He X, Li C, Qian J (2010) Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatr 22: 200-203.
- Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166: 1092-1097. [Crossref]
- Pfizer I (1999) PHQ-9 (Patient Health Questionnaire). Pfizer, New York.
- Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16: 606-613. [Crossref]
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D et al. (2008) Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care 46: 266-274. [Crossref]
- Salari N, Hosseinian Far A, Jalali R, Vaisi Raygani A, Rasoulpoor S et al. (2020) Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systemic review and meta-analysis. Global Health 16: 57. [Crossref]
- Temsah MH, Al Sohime F, Alamro N, Al Eyadhy A, Al Hasan K et al. (2020) The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health 13: 877-882. [Crossref]
- Si MY, Su XY, Jiang Y, Wang WJ, Gu XR et al. (2020) Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty 9: 113. [Crossref]
- Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D et al. (2004) Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med 66: 938-942. [Crossref]
- Lai J, Ma S, Wang Y, Cai Z, Jianbo Hu et al. (2019) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 3: e203976. [Crossref]
- Department of Health, Republic of South Africa, National COVID-19 daily report.
- Imai T, Takahashi K, Hasegawa N, Lim MK, Koh D (2005) SARS risk perceptions in healthcare workers, Japan. Emerg Infect Dis 11: 404-410. [Crossref]
- Phua DH, Tang HK, Tham KY (2005) Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad Emerg Med 12: 322-328. [Crossref]
- Wong WCW, Wong SYS, Lee A, Goggins WB (2007) How to provide an effective primary health care in fighting against severe acute respiratory syndrome: the experiences of two cities. Am J Infect Control 35: 50-55. [Crossref]
- Wang RQ, Hay M, Clarke D, Menahem S (2014) Associations between knowledge of disease, depression and anxiety, social support, sense of coherence and optimism with health-related quality of life in an ambulatory sample of adolescents with heart disease. Cardiol Young 24: 126-133. [Crossref]
- English P, Friedman E, McKeown H, Rao M, Sethi S et al. (2020) Risk Stratification tool for Healthcare workers during the CoViD-19 Pandemic; using published data on demographics, co-morbid disease and clinical domain in order to assign biological risk. medRxiv.
- Mo Y, Deng L, Zhang L, Lang Q, Liao C et al. (2020) Work stress among Chinese nurses to support Wuhan in fighting against COVID‐19 epidemic. J Nurs Manag. [Crossref]
