Rare Case of Gallbladder Perforation in Pediatric Patient: A Pitfall in Generalized Peritonitis in Late Presented Typhoid Fever
A B S T R A C T
An 11-year-old boy presented to the emergency room with generalized abdominal pain, inability to pass gas nor stool in 2 days, along with stepladder pattern fever which he had been having in the past 2 weeks before being admitted to the hospital. Abdominal surgical complications are one of most common complications (10-15% of typhoid fever patients) in pediatric typhoid fever, but gallbladder perforation is an uncommon one. Emergency surgical exploration with cholecystectomy was initiated and showed satisfying outcome [1].
Keywords
Pediatric gallbladder perforation, typhoid fever
Introduction
Gallbladder perforation is a rare complication of cholecystitis, especially in typhoid fever, a fever caused by gram-negative bacteria; Salmonella typhi, which may cause an acute acalculous cholecystitis. Typhoid fever or the so-called enteric fever has become global burden, especially in developing countries, where delayed treatments can still be found in some cases. There are no specific guidelines for managing the abdominal complication, moreover the gallbladder perforation of typhoid fever yet, because of its rare occurrence. Generalized peritonitis in patients with enteric fever may be differentially diagnosed with perforated intestine, intestinal hemorrhage, and rarer cases of perforated gallbladder and appendicitis. We report a case of pediatric gallbladder perforation found during surgical exploration which was presented as generalized peritonitis and at first diagnosed with perforated appendicitis or perforated small intestine [1-3].
Case Report
An 11-year-old boy was presented to Dr. Ramelan Naval Hospital, Surabaya with a chief complaint of generalized abdominal pain and distention starting from 2 days prior to hospital admission. He also complained of right lower quadrant abdominal pain 2 days before. He had not passed stools for the last 2 days, had bilious vomiting and a history of occasional fever over 2 weeks. He had not been admitted to any doctors or hospitals before because of financial reason, therefore he had not received any antibiotics, either.
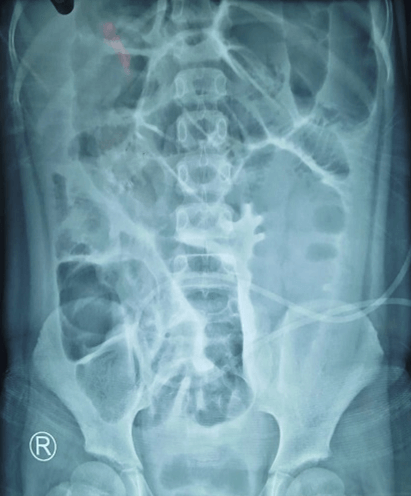
Figure 1: Plain abdominal X-ray.
Vital signs at the time of admission were: blood pressure – 90/65, pulse rate – 128/ minute, temperature – 380C, and respiratory rate – 24 breaths/ minute. On examination, he was not icteric, the abdomen was slightly distended, lowered peristaltic sound and generalized abdominal muscle guarding with abdominal pain particularly in right lower quadrant. Plain abdominal X-ray showed dilated intestine, coiled-spring sign, thickened intestine wall and opacity in the upper right and lower left quadrant. The X-ray is shown in (Figure 1).
His laboratory results showed increased hematocryte, leukocytosis of 19190 u/l, neutrophilia, hyponatremia, and hypokalemia. His Tubex result came after his surgery and resulted positive (+6). The pathological anatomy examination of the gallbladder showed gallbladder with mononuclear inflammation cells infiltration of the lamina propria, Rockitansky aschoff sinus with necrotic area of the muscularis layer with no sign of malignancy, concluded as cholecystitis with hemorrhagic infarct.
Treatment
He was diagnosed with generalized peritonitis and mild to moderate dehydration, which then was given a fluid resuscitation in the emergency ward, along with electrolyte correction while preparing for the surgical exploration.
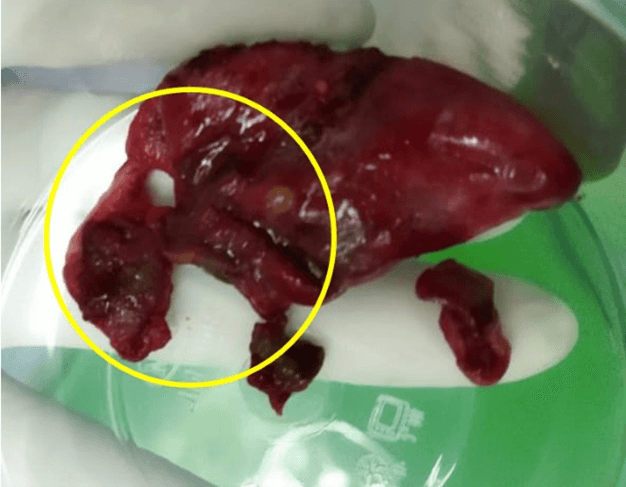
During the operation, the peritoneal fluid was found mixed with pus, dilated – hyperemia of the intestine, especially on the ileum. The appendix was found hyperemia with no perforation. We explored the upper quadrant, discovered parts of intestine near the liver covered in slough, and revealed a perforated of the gallbladder fundus (may be seen in Figure 2). There was no gallbladder stone found in the common bile duct, nor the cystic duct. We decided to do cholecystectomy and appendectomy because of the inflamed appendix which seemed to occur secondarily to the perforation. The peritoneal cavity was lavaged until the peritoneal fluid became clear and put in an intraperitoneal drain in the Morrison’s pouch.
Figure 2: Perforated gallbladder.
After the finding of gallbladder perforation and based on the Tubex result, our patient was given therapeutic antibiotic of thiamphenicol for 7 days, nil per os for 3 days (while given total parenteral nutrition), and maintenance fluid. Patient was then discharged at day 7 post-surgery with no fever, and unrestricted diet. The peritoneal drain was taken off after 10 days.
Discussion
In developing countries, typhoid fever is a common infection mainly caused by Salmonella typhi, found in the environment with poor sanitation and little supply of clean drinking water. It accounts for nearly 27 million cases worldwide and 200000 deaths per year, while in Indonesia the prevalence is 0.3-3%, with highest incidence found in East Java based on 2007. Indonesian Health Research [4, 5].
Acute acalculous cholecystitis which causes the gallbladder perforation in pediatric typhoid fever is not extremely rare, but late presentation in patient may become a pitfall in preoperative diagnosis because of the sign of peritonitis mimicking other causes of peritonitis, such as perforation caused by appendicitis which is the most cause of acute abdominal pain in children [4, 6].
Table 1: Niemeier’s classification of gallbladder perforation
[4].
|
Type |
Onset |
Explanation |
|
Type 1 |
Acute |
Involves perforation of
the gallbladder into the peritoneal cavity; it is not surrounded by any
protective adhesions |
|
Type 2 |
Subacute |
Consists of a perforated
gallbladder surrounded by an abscess that is walled off by adhesions |
|
Type 3 |
Chronic |
Includes the formation of
a fistula between the gallbladder and some viscera |
In this patient, we found type 2 perforated gallbladder based on Niemeier’s classification (Table 1). The treatment of the perforated gallbladder is cholecystectomy continued with peritoneal lavage to manage peritonitis which are usually sufficient, continued with antibiotics. Even though, cholecystectomy in type 3 gallbladder perforation may be difficult. In this case, we preferred thiamphenicol (group of chloramphenicol) because based on the research done in Malang, East Java by Ni Made Diah et al. showed that chloramphenicol was the most cost-effective antibiotic for typhoid fever, compared to ceftriaxone and cefixime both in pediatric patients [4, 7].
Conclusion
Perforated gallbladder in pediatric patient who’s suspected with typhoid infection should be considered in the presentation of peritonitis because even though it is very rare, but acalculous cholecystitis is not an uncommon abdominal complication in pediatric population. Therefore, it should be considered for the surgical approach and choice of abdominal incision, so that surgeons may explore liver region. Cholecsytectomy, peritoneal lavage and peritoneal drain insertion, continued with antibiotic treatment for typhoid infection give a satisfying result.
Article Info
Article Type
Case ReportPublication history
Received: Wed 24, Mar 2021Accepted: Wed 28, Apr 2021
Published: Mon 24, May 2021
Copyright
© 2023 Ageng Budiananti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2021.01.03
Author Info
Ageng Budiananti Sapta Prihartono
Corresponding Author
Ageng BudianantiResident of Pediatric Surgery, Dr. Soetomo General Academic Hospital, Airlangga University, Jawa Timur, Indonesia
Figures & Tables
Table 1: Niemeier’s classification of gallbladder perforation
[4].
|
Type |
Onset |
Explanation |
|
Type 1 |
Acute |
Involves perforation of
the gallbladder into the peritoneal cavity; it is not surrounded by any
protective adhesions |
|
Type 2 |
Subacute |
Consists of a perforated
gallbladder surrounded by an abscess that is walled off by adhesions |
|
Type 3 |
Chronic |
Includes the formation of
a fistula between the gallbladder and some viscera |
References
1.
Chukwubuike KE
(2020) Profile of Abdominal Surgical Complications of Enteric Fever in Children
in a Developing Country. SJMS 15: 270-280.
2.
Yagnik VD (2017)
Type II perforation of the body of the gallbladder in acute acalculous
cholecystitis: a rare complication of enteric fever. IJMU 12: 10-12.
3.
Mehrabani S
(2020) Acute Appendicitis Associated With Typhoid Fever: A Case Report and
Review of Literature. J Pediatr Rev 8: 255-260.
4.
Malik MN, Mahmood T, Din ATU, Aslam S, Imtiaz M (2019)
Gallbladder Perforation Secondary to Enteric Fever: An Interesting Case of
Acute Abdomen. Cureus 11: e4516. [Crossref]
5.
Dewi NMDP, Illahi
RK, Lyrawati D (2019) Cost - Effectiveness Analysis of Chloramphenicol,
Ceftriaxone and Cefixime Use in Pediatric Thypoid Fever Patient.
Pharmaceutical J Indones 5: 53-59.
6.
Leung AKC,
Sigalet DL (2003) Acute abdominal pain in children. Am Fam Physician 67:
2321-2326. [Crossref]
7.
Derici H, Kara C, Bozdag AD, Nazli O, Tansug T et al. (2006) Diagnosis
and treatment of gallbladder perforation. World J Gastroenterol 12:
7832-7836. [Crossref]
