Rare Emergency Case of Bowel Ischaemia as a Result of Diabetic Ketoacidosis Complication: A Case Report and Literature Review of an Unusual Entity
A B S T R A C T
Introduction and Importance: Diabetic ketoacidosis (DKA) is a life-threatening situation that if inadequately managed, is related to high fatality risk. It is associated with mesenteric ischaemia that necessitates early detection and intervention to enhance the prognosis for mesenteric ischaemia.
Case Presentation: A 58-year-old male patient presented to our hospital with severe generalized abdominal pain, vomiting, and polyurea. On admission, he was newly diagnosed with diabetes mellitus type II (DM II) which is complicated by DKA. Days later, his abdominal pain worsened, and bowel obstruction was confirmed by both X-ray and ultrasonography of the abdomen. Due to the deterioration in the patient’s clinical condition, an emergent diagnostic laparoscopy was decided which was followed by an open laparotomy with bowel resection of the detected dilated and ischaemic bowel loops. The resected specimens, including small bowel and peritoneal wall mass, were sent for histopathological studies. Three re-look laparotomies were also performed, and the postoperative period was uneventful.
Clinical Discussion: Intestinal ischaemia is a rare complication of DKA. Bowel ischaemia can be either occlusive or nonocclusive mesenteric types. It is clinically manifested by abdominal symptoms in diabetic patients. Evaluation is mainly by abdominal computed tomography (CT) and the main treatment approach is laparoscopy and/or laparotomy in combination with resection of the affected bowel loops.
Conclusion: In our case report, we document an additional unusual case of intestinal ischaemia and necrosis as a DKA consequence, in a recently diagnosed DM II patient, as one of the few non-occlusive mesenteric ischaemia causes.
Keywords
Bowel ischaemia, diabetic ketoacidosis, small bowel resection, non-occlusive mesenteric ischaemia, laparotomy, case report
Introduction
Diabetes ketoacidosis (DKA) is one of the most serious complications of diabetes mellitus (DM) [1]. DKA occurs more frequently in the pediatric population with diabetes type 1 but is less likely in type 2 DM, accounting for 34% [2]. Contrary to the pediatrics, the literature reported few cases of bowel ischaemia related to DKA in type 1 DM in the adult population, and limited similar cases were documented in the adults with type 2 DM [3]. Non-occlusive mesenteric ischaemia (NOMI), which is a type of bowel ischaemia, is a rare complication of DKA associated with abdominal conditions, bowel necrosis, and sudden hypovolemia, leading to significant morbidity and mortality rates [1, 4].
As a result of hypoperfusion, bowel infarction or gangrenous bowel causes irreversible intestinal damage. Infection and death can result from this condition, which is considered a medical emergency [2]. Here we highlight a 58-year-old gentleman, with no past medical history, who presented with severe abdominal pain found to be due to DKA-related bowel ischaemia. Our work has been reported in line with the SCARE Guidelines 2020 criteria [5].
Case Presentation
A 58-year-old male patient, with no past medical history, presented to our hospital with severe generalized abdominal pain, repeated vomiting, and polyurea. At this point, the patient was diagnosed with type 2 DM which was complicated with DKA. Two days later, the patient’s abdominal pain worsened, localized in the right lower quadrant associated with fever, obstipation, and periumbilical tenderness.
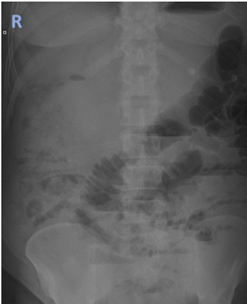
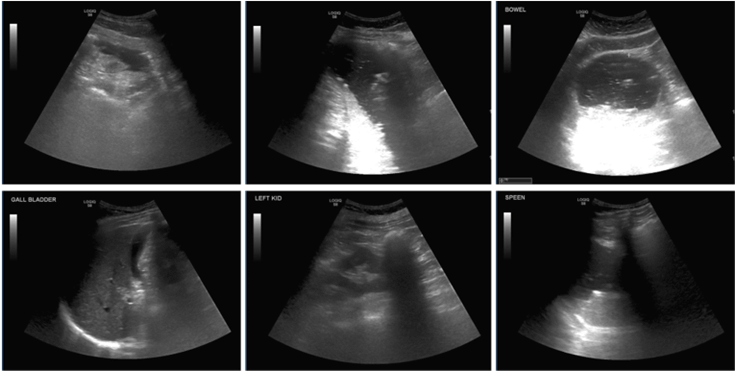
The physical examination showed a conscious, alert, and oriented patient on admission. Abdominal examination revealed a markedly distended abdomen associated with periumbilical tenderness. Laboratory investigations of the patient are mentioned in (Table 1). An abdominal X-ray was done, showing a dilated small bowel (Figure 1). Abdominopelvic ultrasonography showed marked colonic gaseous distention, dilated gut loops were noted in the abdomen up to 5.7 cm, and minimal free fluid in the pelvis (Figure 2).
Figure 1: Abdominal X-ray showed dilated small bowel loops.
Table 1: Patient’s vital
signs and laboratory investigations on admission.
|
Patient’s vital
signs |
Hematology |
Coagulation |
|
GCS 15/15 |
WBC 16.9 |
PT 11.6 |
|
BP 110/70 mmHg
|
Hb 157 |
PT-INR 1.00 |
|
HR 76 bpm |
Platelets 238 |
APTT-A 20.3 |
|
RR 20 bpm |
Neutrophils 13.29 |
APTT-A
Ratio 0.78 |
|
SPO2
99 % on room air |
Lymphocytes 2.55 |
Amylase 107 |
|
Body
temperature 37 o C |
Monocytes 1.00 |
Albumin 46.1 |
|
Lactate
venous plasma 2.76 |
Eosinophils 0.02 |
ALT 17 |
|
PCT 48.03 |
Basophils 0.08 |
AST 54 |
|
CK 981 |
LDH 1120 |
ALK-PHOS 150 |
|
Urea-
17.69 |
Creatinine-
334 H |
GFR-
17 |
Figure 2: Dilated bowel loops illustrated by the abdominopelvic ultrasonography.
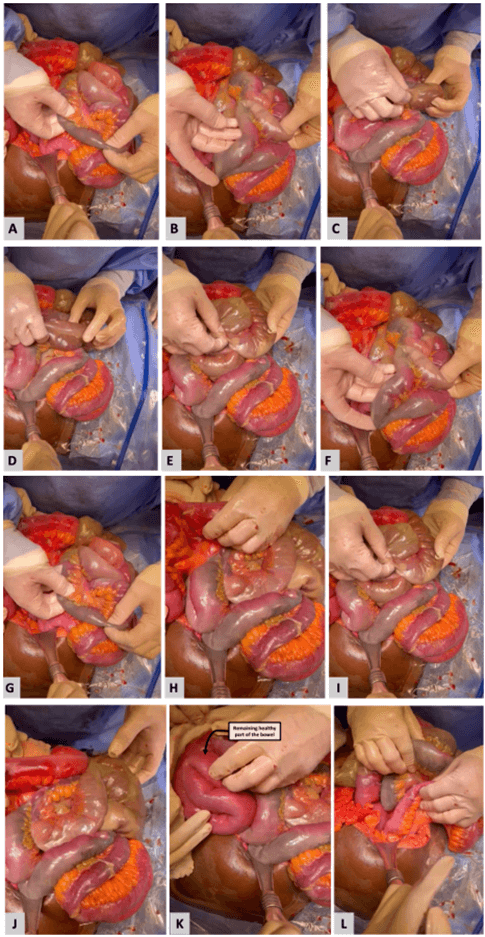
An emergent diagnostic laparoscopy was performed, showing dilated and ischaemic bowel loops with bloody fluid and resulting in bowel resection. Then, the laparoscopic procedure was converted to open laparotomy, which was the first-look laparotomy, that revealed an ischaemic segment of the small bowel involving a 5 cm distal terminal ileum and patchy ischaemic segment from the duodenojejunal junction (DJ). Multiple resections of the bowel were done, and the abdomen was kept open. Examination and washing of the abdominal cavity was done bedside in the ICU. The remaining healthy bowel loops were 25 cm from the DJ, 175 cm in between segments, and 75 cm from the ileocecal valve. Then, side-to-side anastomosis and closure of the abdomen were achieved (Figure 3 intraoperative images).
Figure 3: Intraoperative findings, showing A, C, D & J) gangrenous bowel parts. B) Terminal ileum. E) Gangrenous bowel, only serosa remaining non-ischaemic. F) Septic part of the bowel. L) Approx 50 cm from the duodenojejunal junction is ischaemia-free.
Two days later, a second-look laparotomy and small bowel resection were performed, including a re-evaluation of the small bowel that was started by irrigation and washing. No new ischaemia was noticed in the small bowel and the drainage tube was fixed in the blind loop.
Three days later, a third-look laparotomy was done, and healthy bowel loops and minimal adhesiolysis of the small intestine were intraoperatively detected. Additionally, side-to-side anastomosis at both the duodenojejunal junction and the ileocecal junction was carried out. During the re-look procedure, continuous washing with normal saline and metronidazole was done, hemostasis was maintained, and the abdomen was closed.
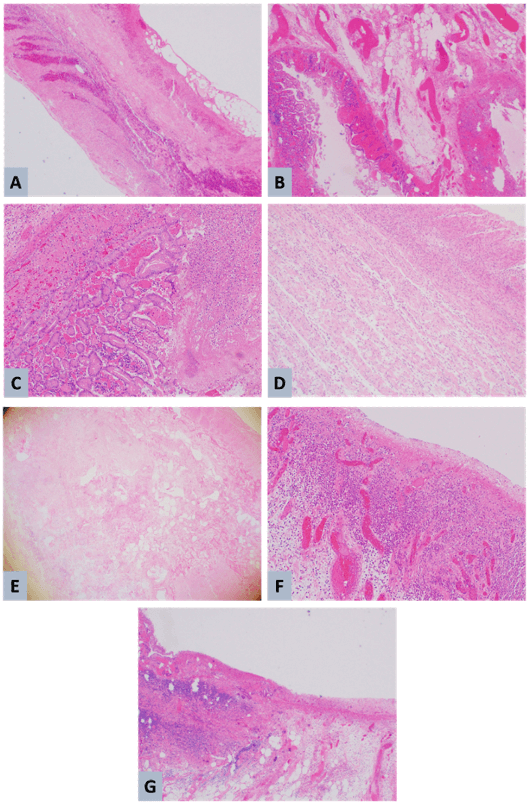
The surgically excised specimen was composed of small bowel tissues and the peritoneal wall mass was sent for histopathology studies. The histopathology study reported acute bowel transmural ischaemic changes, serositis, peri-intestinal fat with hemorrhage and congested vessels, and ischaemic changes in the resected bowel segment margins. Also, it revealed that the resected peritoneal wall mass was a combination of hemorrhagic and fatty tissue (Figure 4).
Then, the patient was clinically improving, the postoperative period was uneventful, and the patient was discharged on postoperative day thirteen.
Figure 4: Histopathological study of the resected specimen of the resected specimen. A) Mural necrosis. B) Transmural necrosis, neutrophils, hemorrhagic infraction. C & D) Transmural necrosis, neutrophils. E) Transmural necrosis. F & G) Mucosal necrosis.
Discussion
Since diabetes mellitus (DM) is considered a hypercoagulable condition, it is extensively investigated [1]. Patients with diabetes are at risk of developing DKA as a feature of poor-controlling DM. DKA is an inflammatory process that is associated with a reduction in proteins C and S and enhancement of von willebrand factor activities, initiating a pro-thrombotic situation [1, 3]. Further studies demonstrated that diabetic patients had elevated levels of clotting factors and aggregated platelets [1]. Due to DM-related epithelial vascular abnormalities, the risk of developing thromboembolic events is documented [1].
According to the reported cases in the literature, the initial presenting clinical feature of DKA is bowel ischaemia, during which DKA fails to respond to treatment by fluid resuscitation to resolve acidosis [1]. Few cases in the literature reported DKA-related mesenteric bowel ischaemia in long-standing type 1 DM. In the current case, the abdominal symptoms did not improve with the DKA treatment protocol, raising suspicion of bowel ischaemia [1]. Ischaemic bowel and DKA relation is a life-threatening situation that is related to high morbidity and mortality rates [1]. This relationship can irreversibly damage the bowel through hypoperfusion, leading to infarcted and/or gangrenous bowel loops [3].
The resultant bowel ischaemia can be due to primary vascular factors. These include mesenteric ischaemia and bowel obstruction causes [2, 3]. Multiple etiologies are related to disturbed perfusion of the small bowel wall, which can be classified into acute, including occlusive and non-occlusive mesenteric ischaemia, and chronic causes [2]. One of the acute occlusive mesenteric ischaemia reasons that is related to 75% of the cases is superior mesenteric artery occlusion, while the occlusion of the superior mesenteric vein is associated with up to 10 % of the cases [2]. NOMI is defined as intestinal ischaemia that is driven by vascular narrowing in the absence of organic mesenteric artery obstruction [6].
The non-occlusive mesenteric ischaemia (NOMI) can be manifested in traumatic abdominal injuries, systemic hypotension, and vasoconstriction induced by medication [2, 3]. Small bowel obstruction is additionally involved in the NOMI component [2]. Atherosclerotic superior mesenteric artery stenosis, which may trigger mesenteric angina, and chronic radiation enteritis are instances of chronic etiologies [7]. In the reported case, small bowel obstruction was the underlying cause of NOMI, leading to bowel ischaemia. Due to the absence of identifiable manifestations and clinical examination results, it is still a disorder that is undetected and underestimated [8]. Gocho et al. documented that the early signs and symptoms of NOMI, such as abdominal pain, nausea, vomiting, tiredness, weakness, and disorientation are not specific, thus it can be challenging to make a rapid diagnosis. This makes NOMI fatalities extremely prevalent [6, 8].
The diagnostic guidelines for NOMI are still not identified [8]. Due to its rapidity, non-invasiveness, and high level of accuracy, CTA is an initial imaging approach [1, 3, 9]. As early detection can significantly increase the chance of intestinal salvage, the treating physician should have a low threshold for performing a CTA abdomen and pelvis for early diagnosis [10]. In our case, the abdominal CT with intravenous and oral contrast was planned but not performed due to the patient’s instability.
DKA and unregulated hyperglycemia rarely result in intestinal ischaemia [11]. The presented case is one of the few that, to our knowledge, demonstrated an effective treatment of DKA-induced ischaemia of the intestine due to prompt surgical action [11]. Revascularization of the tissue with ischaemia and resection of the necrotic bowel are the principal objectives of management [3, 6]. Our patient was managed surgically by laparotomy and bowel resection with intraoperative details mentioned in the case presentation section.
Conclusion
DKA is a medical emergency and its complications have high morbidity and mortality rates. These complications are usually misdiagnosed and early diagnosis and management of such cases are crucial for life saving. The current case reported an unusual presentation of a newly diagnosed NIDDM adult patient who was admitted with a clinical picture of DKA that was rapidly complicated with bowel ischaemia. Documentation of such cases is highly encouraged to improve the outcomes of this life-threatening situation.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
Not applicable.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author Contributions
Athary Saleem: Assisted in surgery, paper writing and editing, picture editing, and manuscript drafting. Saqer Alenezi: Literature review, paper writing, and editing. Jumana Alfadhli: Assisted in surgery, and paper editing. Fahad Alhammadi: Paper editing. Maher Hassan: Performed surgery, and paper editing. Khaled Alshammari: Performed surgery, critical review, picture editing, supervision, and final approval.
Guarantor
Athary Saleem, D. Pharma., B. Med. Sc., M.D., General Surgery Department, Al-Adan Hospital, Kuwait.
Research Registration
Not applicable.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Fri 10, Nov 2023Accepted: Mon 11, Dec 2023
Published: Sat 30, Dec 2023
Copyright
© 2023 Athary Saleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2023.04.02
Author Info
Athary Saleem Saqer Alenezi Jumana Alfadhli Fahad Alhammadi Maher Hassan Khaled Alshammari
Corresponding Author
Athary SaleemNeurosurgery Department, Jaber Al Ahmad Hospital, State of Kuwait
Figures & Tables
Table 1: Patient’s vital
signs and laboratory investigations on admission.
|
Patient’s vital
signs |
Hematology |
Coagulation |
|
GCS 15/15 |
WBC 16.9 |
PT 11.6 |
|
BP 110/70 mmHg
|
Hb 157 |
PT-INR 1.00 |
|
HR 76 bpm |
Platelets 238 |
APTT-A 20.3 |
|
RR 20 bpm |
Neutrophils 13.29 |
APTT-A
Ratio 0.78 |
|
SPO2
99 % on room air |
Lymphocytes 2.55 |
Amylase 107 |
|
Body
temperature 37 o C |
Monocytes 1.00 |
Albumin 46.1 |
|
Lactate
venous plasma 2.76 |
Eosinophils 0.02 |
ALT 17 |
|
PCT 48.03 |
Basophils 0.08 |
AST 54 |
|
CK 981 |
LDH 1120 |
ALK-PHOS 150 |
|
Urea-
17.69 |
Creatinine-
334 H |
GFR-
17 |
References
1. Vivino GR, Crofton
NA, Mussarat S (2022) Diabetic Ketoacidosis and Acute Mesenteric Ischemia in
Adults: An Underreported Association. Cureus
14: e29053. [Crossref]
2. Kishman AM,
Stanoeva J, Josev AP (2022) Small Intestine Necrosis Presented as acute Abdomen
in Elderly Diabetic Type 2 Patient. Albanian
Journal of Trauma and Emergency Surgery 6: 982-985.
3. Esper L (2021)
Mesenteric Ischemia in a Young Man With the First Presentation of Diabetic
Ketoacidosis. J Endocr Soc 5: A392. [Crossref]
4. Silva M, Gounder V
(2022) Recurrent bowel necrosis from non-occlusive mesenteric ischemia induced
by diabetes ketoacidosis in an adult patient causing mortality: a rare cause of
mortality associated with poorly controlled diabetes in adults. International Surgery Journal 9: 2051-2054.
5. Agha RA, Franchi T,
Sohrabi C, Mathew G, Kerwan A (2020) The SCARE 2020 Guideline: Updating
Consensus Surgical CAse REport (SCARE) Guidelines. International Journal of
Surgery 84: 226-230. [Crossref]
6. Itoh Y, Sagawa R,
Kinoshita H, Tamba S, Yamamoto K et al. (2019) Small-intestinal necrosis due to
non-occlusive mesenteric ischemia with diabetic ketoacidosis after quetiapine
treatment. Diabetol Int 10: 225-230. [Crossref]
7. Vinod VC, Farhana
U, Waring S, Mlawa G (2022) A Rare and Interesting Presentation of Diabetic
Ketoacidosis Caused by Native Aortic Valve Endocarditis Complicated by Aortic
Root Abscess Resulting in Multiple Septic Emboli Causing Bowel Ischemia and
Splenic Infarction. Cureus 14: e29254. [Crossref]
8. Gocho N, Aoki E,
Okada C, Omura K, Hirashima T et al. (2016) Non-occlusive mesenteric ischemia
with diabetic ketoacidosis and lactic acidosis following the administration of
a sodium glucose co-transporter 2 inhibitor. Intern Med 55:
1755-1760. [Crossref]
9. El Reshaid K, Al
Bader D (2017) Symptomatic thrombosis of superior mesenteric vein due to
diabetic ketoacidosis. Int J Med Res Prof
3: 263-265.
10. Hohmann C, Teuteberg S, Aschenbrenner I, Kaag N, Heizmann O (2019) Non-occlusive Mesenteric Ischemia caused by Diabetic Ketoacidosis-Pneumatosis intestinalis and Portal Venous Gas as an Indication of Mesenteric Ischemia. Dtsch Med Wochenschr 144: 1638-1641. [Crossref]
11. Park JH, Muncie C, Sawaya Jr DE (2022) Intestinal ischemia resulting in enterectomy in poorly controlled type 1 diabetes mellitus with diabetic ketoacidosis. Journal of Pediatric Surgery Case Reports 82: 102309.
