Confluent and Reticulated Papillomatosis of Gougerot and Carteaud in Two Identical Twins: Case Report
A B S T R A C T
Confluent and reticulated papillomatosis of Gougerot-Carteaud (CARP) is a rare dermatosis. Even though many authors affirm that it is a keratinization disorder, the causes are still unknown. There are various therapeutic options to treat this disorder: retinoids, antibiotics, keratolytic, and others, but the results are unsatisfactory. This study presents the case of two identical twins, approaching clinic characteristics, as well as histopathologic characteristics, and the difficulties of finding the correct diagnosis since it is a rare disease.
Keywords
Hyperpigmentation, keratosis, skin diseases
Introduction
Confluent and reticulated papillomatosis is a rare dermatosis, originally described by Gougerot and Carteaud in 1927. It is characterized by hyperpigmented papules, that can coalesce into plaques to form a reticular pattern peripherally and confluent plaques centrally. It is a rare dermatosis which is more frequently found in women and melanodermic subjects, with higher incidence between the ages of 10 and 35 years [1]. It is rarely symptomatic and typically distributed around the neck, interscapular region, infra-mammary area, back and the abdomen [2]. Dermatoscopic evaluation can observe fine whitish scaling and brownish flat polygonal globules separated by pale striae, creating a cobblestone pattern (Dermatoscopy of confluent and reticulated papillomatosis, 2017). Davis et al. proposed five criteria for the diagnosis of confluent and reticulated papillomatosis: (i) clinical findings of scaling brown macules and patches, part of which appear reticulated and papillomatous (ii) involvement of the upper trunk and neck (iii) fungal staining is negative for fungus (iv) no response to antifungal treatment (v) excellent response to minocycline [3].
The histology of the disease demonstrates epidermal undulation with hyperkeratosis, papillomatosis and minimal acanthotic downward projections from the bases of the dells between the papillomatous areas [4]. Various treatment modalities have been proposed, but the studies have been inconsistent. Currently, the use of antibiotics, especially minocycline and other macrolides have been reported to be highly effective in these patients [2]. The effectiveness may be due to anti-inflammatory rather than antimicrobial effects alone. Systemic retinoids, topical therapies such as topical retinoids, urea, calcipotriol and tacrolimus have been successful, but the antibiotics are still preferred [5].
Case Presentation
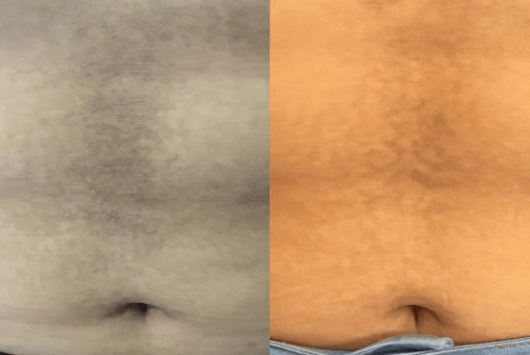
Two 18-years-old identical twins presented to the Dermatology Department with a three-year history of flat brown skin papules and peeling of surface layers, which coalesced to form diffuse large confluent plaques centrally and a reticular pattern peripheral, spread out the medial abdomen (Figures 1 & 2). Mild pruritus was also present. They have done previous treatment with topical use of Ketoconazole and systematic treatment with Fluconazole 150 mg (1 pill per week for 2 months), with no clinical results. Physical exam confirmed papular lesions, brownish, keratotic, and peeling surface, confluent in the middle, forming plaques of growing evolution on the abdomen. Considered diagnosis were Acanthosis Nigricans, Pityriasis Versicolor and Confluent and Reticulated Papillomatosis of Gougerot-Carteaud (CRP).
Figure 1: Patient 1, A) Hyperchromic, keratotic papules in plaques on the abdomen. B) After three months, recovery of lesions on hyperchromic and residual hypochromic areas.
Figure 2: Patient 2, A) Hyperchromic, keratotic papules in plaques on the abdomen. B) After three months, recovery of lesions on hyperchromic and residual hypochromic areas.
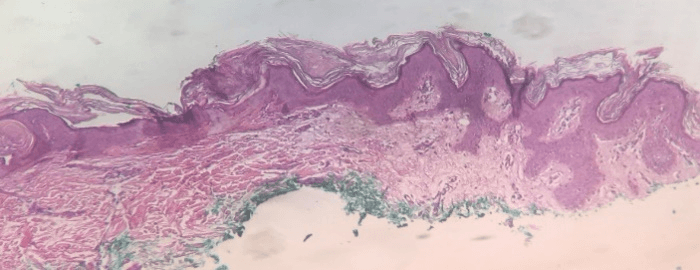
Incisional biopsy of the abdominal injury was performed under local anesthesia, with vasoconstrictor solution. Samples of the injured area were obtained with a punch number 4, reaching deeper layers, including hypodermis. Histopathological analysis of lesions in both patients showed hyperkeratosis (vacuolated as well as compact), mild acanthosis and not strict papillomatosis. Absence of hyperpigmentation on the basal layer and negative PAS histochemical technique for fungus on stratum corneum. Therefore, a hyperkeratosis, epidermal hyperplasia and papillomatosis was confirmed (Figures 3 & 4).
Figure 3: Patient 1: Epidermis with compact hyperkeratosis, mild papillomatosis, and mild acanthosis. Normal dermis (Hematoxylin and Eosin 100X).
Figure 4: Epidermis with hyperorthokeratosis, mild papillomatosis, and mild acanthosis. Normal dermis (Hematoxylin and Eosin 100X).
Direct mycological exam and culture for fungus were negative. Laboratory exams and serological tests have not shown changes, which discards the possibility of endocrinopathies and atopy. The differential diagnosis includes acanthosis nigricans, however, this possibility was excluded by the fact that this disease is mainly in intrigue areas, such as underarm and neck. Versicolor Pityriasis was also ruled out since mycological and histochemical studies and culture are negative. The close correlation between clinical data and histopathological findings confirmed the diagnosis of CRP. In order to treat the presented disease the following medications have been recommended: the topical use of keratolytic, 20% urea-based, 2% salicylic acid, and systemic use of Azithromycin in pulse therapy, 500 mg -once a day for three consecutive days, a pause of 7 days and repeat the 6 times. The patients still under follow-up in the outpatient dermatology clinic, they have been shown gradual progress on the treatment of the lesions.
Discussion
In this study we report two identical twin sisters with CRP diagnosis. Few cases of the disease in the same family between siblings have been reported in the literature [6, 7]. However, no case of identical twin sisters has been reported. CRP is a condition due to disorderly keratinization. The disease was originally described by Gougerot and Carteaud. Its etiology remains uncertain. Pathogenesis of CRP remains unknown but is thought to involve defective keratinization resulting in cutaneous hyperproliferation [8]. Primarily, Malassezia furfur was thought to be the cause of confluent and reticulated papillomatosis, but studies have been inconsistent and the current infection theory is that the dermatosis is caused by bacteria, named Dietzia papillomatosis, an anaerobic gram positive coccus actinomycete [8]. Other possible causes that have been suggested include reaction to UV light, variation of cutaneous amyloidosis and endocrine abnormalities, including diabetes mellitus, obesity. Confirming literature data, our patients were young adults and african descendants. Nevertheless, they had a body mass index under 25 and did not have any endocrine abnormality.
Familial predisposition has been suggested, but the mode of inheritance in these families has not been established in the current studies [9]. This is a disease underdiagnosed especially in black skin and it is very often confused with other dermatosis, like a pigmented form of tinea versicolor. Other differential diagnosis to consider are acanthosis nigricans, Dowling-Degos disease, Galli-Galli disease, dyskeratosis congenital, prurigo pigmentosa and Darier disease [10]. Clinically, the rash is most commonly confused with pityriasis versicolor, acanthosis nigricans and Darie's disease [2]. Both patients had brown desquamative confluent plaques, mainly in the trunk region, as described in most cases in addition to the pruritus, but the greatest discomfort for both patients was mainly aesthetic. Frequently, diagnosis is delayed and the disorder not recognized by physicians, including dermatologists [2, 4].
Diagnosis could be clinical, but a skin biopsy is of pivotal importance to exclude other disorders. Therefore, we decided to investigate the lesions with the surgical biopsy technique, under local anaesthesia with vasoconstrictor added to the anaesthetic, in which small fragments of 4 mm were removed from the epidermis and dermis of both sisters. Histopathological findings were identical in both patients (vacuolated and also compacted hyperkeratosis, mild papillomatosis, and acanthosis) and led us to the diagnosis of CPR, along with the clinical history. Although there is a variety of treatment for the disease in question, oral minocycline 50-100mg twice a day has been the preferred treatment. However, recent reports of the effectiveness of azithromycin 250-500mg three times a week may make this drug the treatment of choice, since it has a more benign adverse effect profile than minocycline [8].
Thinking of such a scientific report, we opted as a therapeutic approach for our patients with 500mg azithromycin pulse therapy. Patients continue to be followed up with the dermatology outpatient clinic, with gradual but significative improvement of the lesions.
Article Info
Article Type
Case ReportPublication history
Received: Thu 07, May 2020Accepted: Tue 09, Jun 2020
Published: Wed 24, Jun 2020
Copyright
© 2023 Thaís Gomes Casali. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.14
Author Info
Maria Isabel Braga Malveira Adriana Martins Dornelas Allen Baia Gualter Leite Aloisio Carlos Couri Gamonal Maria Christina Marques Nogueira Castañon Raquel Quintao e Silva Marchetti Shirley Braga Lima Gamonal Thaís Gomes Casali
Corresponding Author
Thaís Gomes CasaliProfessor of Suprema College of Juiz de Fora, Brazil
Figures & Tables


References
- Ferreira LM, Diniz LM, Ferreira CJM (2009) Confluent and reticulated papillomatosis of Gougerot and Carteaud: report of three cases. An Bras Dermatol 84: 78-81. [Crossref]
- Lee SW, Loo CH, Tan WC (2018) Confluent and reticulated papillomatosis: Case series of 3 patients from Kedah, Malaysia and literature review. Med J Malaysia 73: 338‐339. [Crossref]
- Davis MDP, Weenig RH, Camilleri MJ (2006) Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol 154: 287-293. [Crossref]
- Errichetti E, Maione V, Stinco G (2017) Dermatoscopy of confluent and reticulated papillomatosis. J Dtsch Dermatol Ges 15: 836-838. [Crossref]
- Le C, Bedocs PM (2020) Confluent and Reticulated Papillomatosis. StatPearls Publishing. [Crossref]
- Maja N, Hocar O (2017) Papillomatose confluente et réticulée de Gougerot-Carteaud: à propos dun cas. Pan Afr Med J 26: 207. [Crossref]
- Rietz S, Grabbe S, von Stebut E (2016) Two brothers with confluent and reticulated papillomatosis. J Dtsch Dermatol Ges 14: 1303-1305. [Crossref]
- Scheinfeld N (2006) Confluent and Reticulated Papillomatosis : A Review of the Literature. Am J Clin Dermatol 7: 305-313. [Crossref]
- Berg MH, Pehr K (2017) Familial Confluent and Reticulated papillomatosis in 2 kindreds including 3 generations. J Cutan Med Surg 22: 330-332. [Crossref]
- Ahogo KC, Gbery PI, Bamba V, Kouassi YI, Ecra EJ et al. (2016) Confluent and reticulated papillomatosis of Gourgerot-Carteaud on Black Skin: two observations. Case Rep Dermatol Med 2016: 2507542. [Crossref]
