Rhizarthrosis Bilateral – Trapeziectomy Versus Arthroplasty with Dual Mobility Prosthesis: Case Report
A B S T R A C T
Background: The trapeziometacarpal joint is the second joint affected by osteoarthritis in the hand. The symptoms and clinical presentation are characterized by pain, limited range of motion, muscle weakness with loss of strength, bone deformities and disability. The symptomatology often is not related to the radiographic grade of osteoarthrosis. Therefore, in addition to the radiographic stage of the disease, the treatment is influenced by multiple variables such as age, functional requirement, symptoms and stability of the joint.
Objective: There are several options of surgical treatments. Although trapeziectomy and its technical variation is the gold standard for treatment, prosthesis replacement can be used with good results. This case report discusses the case of a 70-year-old male who presents bilateral trapeziometacarpal osteoarthrosis treated with two different techniques with different timelines.
Methods: The patient underwent a trapeziectomy on the right hand and arthroplasty with implant on the left. In both TMC the stage of the disease was grade III according to the Eaton Litter classification and the results were evaluated according to clinical and radiographic criteria. The NPRS pain scale and the Quick Dash functional scale were used in subsequent checks. The mean follow-up was 12 months.
Conclusion: There were no significantly different results with respect to pain, activities of daily living, mobility or strength. No complications were observed. The patient is satisfied with the treatment having found a better and earlier resumption of daily activity of the left hand treated with prosthesis replacement.
Keywords
Osteoarthrosis, bilateral, trapezium, trapeziectomy, prosthesis, dual mobility
Introduction
Trapeziometacarpal arthrosis is the disease common in the hand and its incidence is elevated and it is only second to interphalangeal ostheoartrosis [1]. The prevalence rates among 30% in women, overtake 57% of population over 60 years of age with greater incidence in the non-dominant hand [2, 3]. The Trapeziometacarpal joint is very important because it carries out actions that are indispensable for daily activities, and a lack of it gives an important disability. Trapeziometacarpal arthrosis is a condition with a significant impact on the quality of life and it can cause worsening symptoms such as activity-related disabling pain, swelling, weakness, reduction of range of motion, deformity, and loss of grip. The patients often complain of discomfort in carrying out normal daily activities such as brushing one’s teeth to opening a bottle of water or turning keys in the lock. The aetiology is multifactorial; many authors believe that ligamentous laxity plays a role, therefore those with an individual predisposition, or connective tissue disease, metabolic diseases and hormonal disorders such as the release of relaxing induced in pregnancy fall into this group [4]. The risk factors include jobs that overload the joint and repetitive microtrauma.
Women are the most inclined to have this pathology. Diagnosis is based on history and clinical presentation. Patients initially present activity-related pain, later pain becomes worse localized at the base of the thumb. Initially we must discriminate between inflammatory pain such as De Quervain syndrome, from tenosynovitis or from arthritic pain. Clinical examination is essential; there are several tests to evaluate rhizoarthrosis, which are the grind test and the traction shift. These tests have a medium sensitivity but a specificity greater than 95% [5]. In advanced stages of the disease, different degrees of deformity will be evident. Three-projections of hand X-ray is imperative for diagnosis, specifically taken in antero-posterior, latero-lateral, and oblique views.
In addition, special radiographic projections such as that described by Robert and revisited by Lewis can be performed [6, 7]. The most used classification system is that of Eaton and Littler which divides the disease into 4 stages with increasing severity taking into consideration the following characteristics: the space of the joint line, the presence of subluxation and the size of the osteophyte [8, 9]. However, it is important to correlate radiographic findings with history and clinical examination because often there is clinical radiological mismatch [10]. The early treatment includes physiotherapy and splinting backed by antalgic therapy. If the symptoms persist, it is advisable to proceed with intraarticular injections of steroid and lately also with hyaluronic acid even if scientific evidence is limited [11, 12]. Surgical treatment is indicated if conservative treatments have failed. Many techniques are used, and the principal ones are: trapeziectomy with or without ligamentoplasty and arthroplasty with implants. The present report describes the case of a 70-year-old male who presents bilateral trapeziometacarpal arthrosis. The reported case shows the use of two different techniques with different timelines and an intervention with trapeziectomy on the right hand and arthroplasty with implant on the left.
Case Presentation
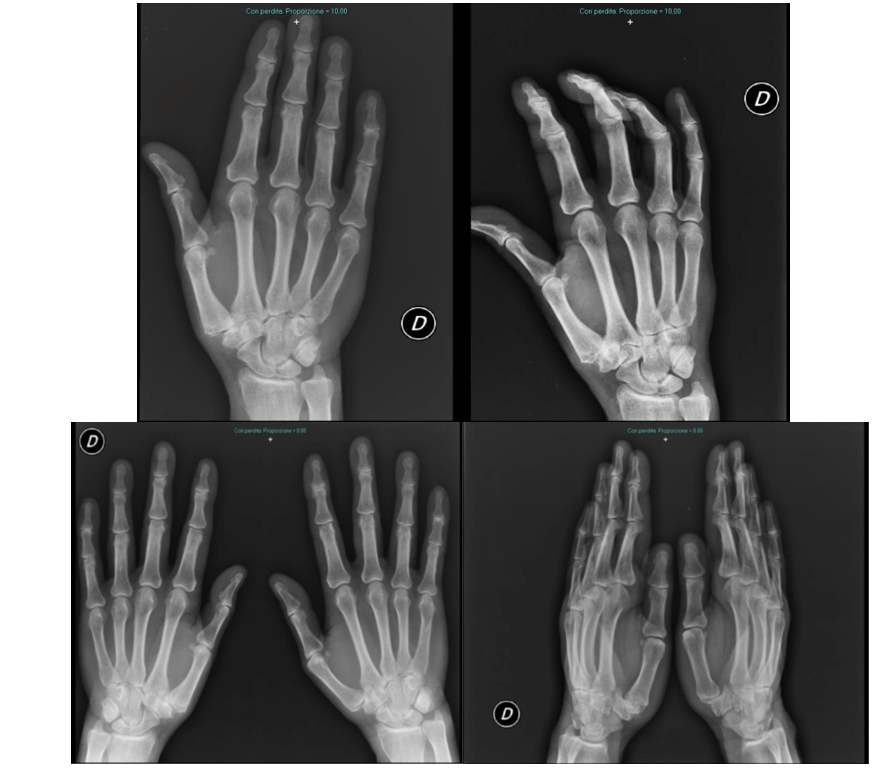
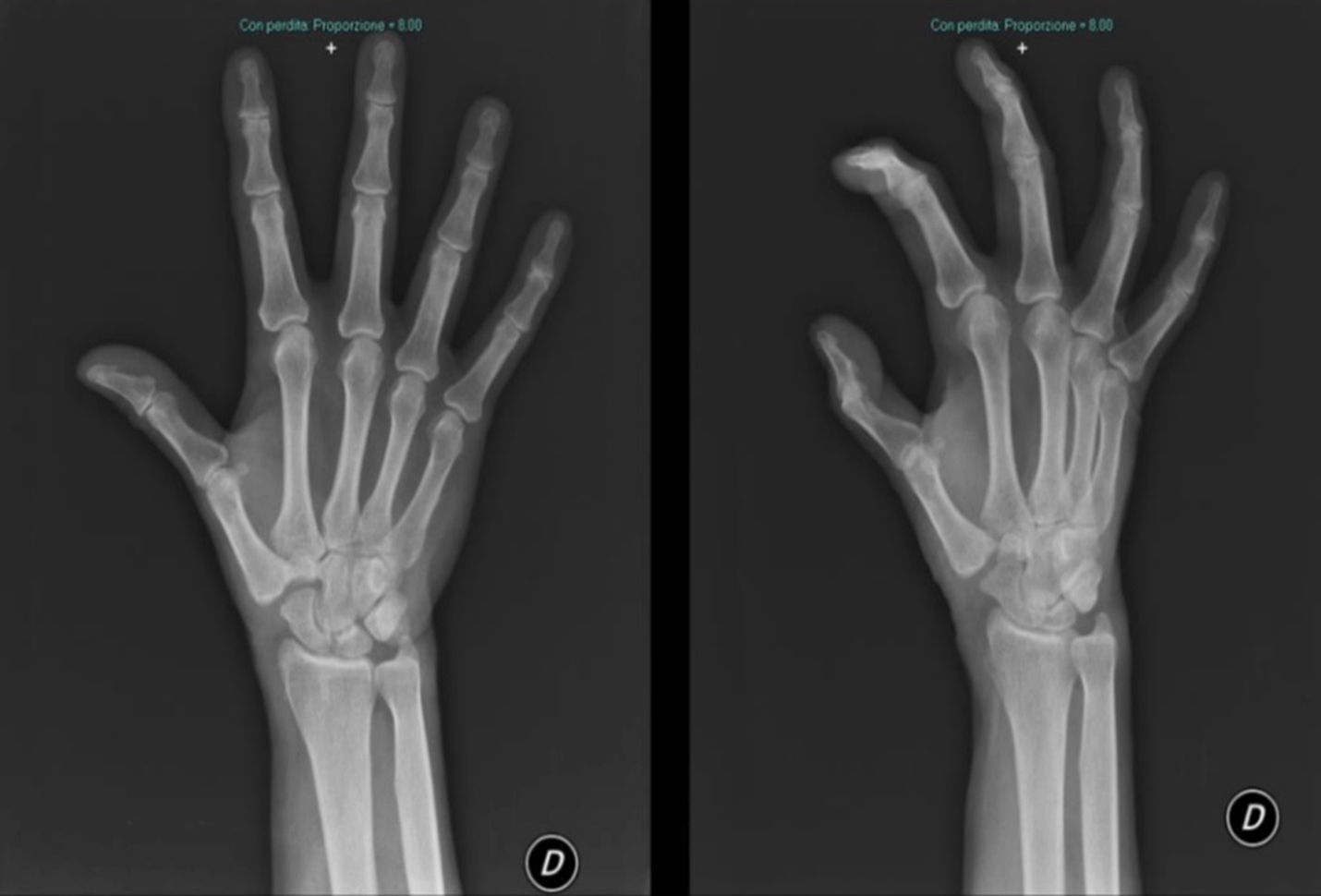
Introducing the case report of a 70-year-old man who came to our attention in 2017, at the “Ospedale Maggiore Carlo Pizzardi” in Bologna, complaining about trapeziometacarpal joint pain and related loss of function of the right thumb. Clinical symptomatology was characterized by activity-related pain and swelling localized at the base of the thumb. Clinical evidence documents positivity of the grind test and the traction shift. X-rays of both hands show bilateral rizharthrosis at third stage according to the Eaton classification (Table 1) [13].
Table 1: Classification of Eaton and Littre.
|
Classification of Eaton and Littre |
|
STAGE I |
|
Normal or slightly widened trapeziometacarpal joint, normal articular contours, trapeziometacarpal subluxation |
|
STAGE II |
|
Decreased trapeziometacarpal joint space, Trapeziometacarpal subluxation, osteophytes or loose bodies less than 2 mm in diameter |
|
STAGE III |
|
Further decreased trapeziometacarpal joint space, subcohondral cysts or sclerosis, trapeziometacarpal joint of one third or more of the articular surface, osteophytes or loose bodies 2 mm or more in diameter |
|
STAGE IV |
|
Involvement of the scaphotrapezial joint or less commonly the trapeziotrapezoid or trapeziometacarpal joint to the index finger |
Contralateral hand symptomatology was not clear, pain was activity related without swelling with positive grind test but negative shift test. Initially treatment was prescribed with physical therapy of both hands and immobilization with dedicated brace of the right thumb mainly because of more pain. After the period of initial benefit, the patient referred to pain persistent on the right hand, thus, he underwent a cycle of intraarticular injections with steroids. Persistence of symptoms and poor benefit from proposed treatment drove the patient to undergo an operative treatment for trapeziectomy of the right hand. After a period of immobilization with brace for two weeks the patient begins physiotherapy for the recovery of the range of motion. The patient was followed regularly at 3-6-12-24 months recording clinical progress according to the QuickDash score questionnaire. The results of the Quick Dash score are shown in (Tables 2 & 3) while the Rx-ray views are shown in (Figures 1-3 & 8).
Table 2: Quick Dash score of right hand: Results with 12 months follow up.
|
Time |
3 months |
6 months |
12 months |
Average |
|
Open a jar |
4 |
3 |
2 |
3 |
|
Do heavy household |
3 |
2 |
2 |
2,33333333 |
|
Carrying shopping bag |
4 |
3 |
1 |
2,66666667 |
|
Wash your back |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
4 |
3 |
3 |
3,33333333 |
|
Impact recreational activities |
4 |
2 |
2 |
2,66666667 |
|
Interference with social activities |
3 |
1 |
1 |
1,66666667 |
|
Work/regular activities |
3 |
1 |
1 |
1,66666667 |
|
Pain |
2 |
1 |
1 |
1,33333333 |
|
Tingling |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
|
QDs |
43,2 |
18,2 |
11,4 |
24,2666667 |
Table 3: Quick Dash score of right hand: Results with 2 year follow up.
|
Time |
3 months |
6 months |
12 months |
2 years |
Average |
|
Open a jar |
4 |
3 |
2 |
2 |
2,75 |
|
Do heavy household |
3 |
2 |
2 |
2 |
2,25 |
|
Carrying shopping bag |
4 |
3 |
1 |
1 |
2,25 |
|
Wash your back |
1 |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
4 |
3 |
3 |
2 |
3 |
|
Impact recreational activities |
4 |
2 |
2 |
2 |
2,5 |
|
Interference with social activities |
3 |
1 |
1 |
1 |
1,5 |
|
Work/regular activities |
3 |
1 |
1 |
1 |
1,5 |
|
Pain |
2 |
1 |
1 |
1 |
1,25 |
|
Tingling |
1 |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
1 |
|
QDs |
43,2 |
18,2 |
11,4 |
9,1 |
20,475 |
Figure 1: X-ray pre operatory of right hand that shows Stage III according to Eaton and Littre classification.
Figure 2: X-Ray of Surgical treatment of trapeziectomy of right hand.
Figure 3: X-Ray post operatory right hand and confront both hands. Follow up 1 year.
One year from the first surgical operation the patient asked to be treated on the increasingly sore left hand at the NPRS 9 (Numeric pain rating scale). Good positive results reported in literature regard arthroplasty with implants of dual mobility trapeziometacarpal prosthesis have encouraged us to apply the patient for this treatment. We opted the for the Touch® by KeriMedical (KeriMedical Switzerland). Post-operative, the hand was immobilized for two weeks with a plaster cast for better patient-supported management. After the removal of the immobilization the patient has immediately started exercise for autonomous functional re-education, showing lesser stiffness and pain than the first operation of the right hand. No early and medium-term complications were observed. Results of the Quick Dash score are shown in (Table 4) and X-Ray views and clinical presentation are shown in (Figures 4-8).
Table 4: Quick Dash score: Results with 12 months follow up in arthroplasty treatment with implant.
|
Time |
3 months |
6 months |
12 months |
Average |
|
Open a jar |
3 |
2 |
1 |
2 |
|
Do heavy household |
3 |
2 |
1 |
2 |
|
Carrying shopping bag |
2 |
2 |
1 |
1,66666667 |
|
Wash your back |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
2 |
2 |
2 |
2 |
|
Impact recreational activities |
3 |
2 |
1 |
2 |
|
Interference with social activities |
3 |
2 |
1 |
2 |
|
Work/regular activities |
3 |
1 |
1 |
1,66666667 |
|
Pain |
1 |
1 |
1 |
1 |
|
Tingling |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
|
QDs |
27,3 |
13,6 |
2,3 |
14,4 |
Figure 4: X-Ray Preoperatory of left hand that shows Stage III according to Eaton and Littre classification.
Figure 5: X-Ray post operatory of left hand.
Figure 6: X-Ray Follow-up 6 months of left hand.
Figure 7: X-Ray Follow-up 1 year of left hand.
Interview and clinical examination of the patient, satisfied for both procedures, has allowed us to highlight a meaningful difference of pinch strength between right and left thumb, both in tip, palmar and lateral pinch tests. In fact, the best results about pinch strength were recorded on the left side treated with arthroplasty with dual mobility prosthesis, despite the function and recruitment of adductor muscles are similar. Another important clinical evidence is moderate shortening of the right thumb, treated with trapeziectomy, resulting in different anatomical attitudes in mild hyperextension of the first metacarpophalangeal joint and different muscle compensation for opposition movement with fifth digit, as showed in the pictures. Analysing the recreational actions, being the patient a retired carpenter he delights during the week in chores. He points out difficulty using the hammer with his right hand, preferring the nondominant hand even for the daily use of a kitchen knife or to open a jar. The degree of subjective satisfaction was comparable between the right and left hand with no significant differences for pain, tingling and difficulty sleeping due to pain. Until the last follow up no complications common to arthroplasty with prosthesis such as synovitis, dislocation, secondary instability, loosening, infection and osteolysis were pointed out [9]. The results of our report document that in the medium-term follow-up (12 months) the difference is considered good for arthroplasty with dual mobility prosthesis and satisfactory for trapeziectomy. Results assessed at 2 years the dash score value is better than 1 year; however, this is not in the good group (Table 5).
Figure 8: Follow-up 1 year. Left Hand that underwent prosthesis replacement was marked.
Table 5: Graded list of QuickDASH score [14, 15].
|
Interpretation |
Score |
|
Very good |
0-5 |
|
Good |
6-15 |
|
Satisfactory |
16-35 |
|
Poor |
>35 |
DASH: Disabilities of the arm, Shoulder and Hand.
Discussion
Treatment of rhizoarthrosis with arthroplasty is a controversy because there are few studies that show its superiority to trapeziectomy either simple or with ligamentoplasty. Prosthetic durability is unpredictable mostly because poorly supported by studies in literature for value rates of complications [16].
At present trapeziectomy without ligamentoplasty is an optimal treatment. However, metacarpal migration with shortening, pain and less straight also demonstrated in biomechanical studies on cadaver, has led surgeons to look for other solutions such as ligamentoplasty, although different studies show no significant differences [17-21]. A variation of trapeziectomy technique is the hematoma distraction arthroplasty with fixing by k wires. This technique apparently has some advantages such as shorter and easier surgical procedure with a less painful recovery, although potential complications related to the fixation with k wires such as irritation, loosening, migration and infections [22]. Despite the logic of distraction some studies do not provide evidence to support the use of temporary K-wire stabilization after trapeziectomy or of the LRTI (ligament reconstruction and tendon interposition) [23]. Therefore, the gold standard for surgical treatment of rhizarthrosis appears to be the trapeziectomy [24]. Patients have pain relief and recovery of movement at about 85%, but without advantages about strength [23]. Even if single case reports do not support the scientific evidence, we consider a good example of comparison of two different surgical techniques still discussed today. In fact, the results of this report help us to understand what the benefits and drawbacks are related to single treatment, each one without complications.
At one year follow up, the Quick Dash scale for the left hand treated with dual mobility prosthesis, showed a lower and therefore better score. The most significant responses were undoubtedly linked to the measurement of daily activities and limited interference of the joint during gripping movements and strong stress on the joint (taking shopping bags, cutting food with a knife). Despite the time elapse since the first trapeziectomy surgery on the right side, two year follow up, the right-handed patient reports more benefits from the arthroplasty with dual mobility prosthesis on the left side, complaining less range of motions of the right thumb, especially of the adduction although greater force. However, trapeziometacarpal arthrodesis is to be considered a final surgical option. It presents more complications respect trapeziectomy with ligament reconstruction and it represents an indication of choice for revision procedures [25]. It is not indicated in manual workers and professionals or who require greater flexibility of the thumb [26]. In relation to the patient’s functional demands, we felt arthrodesis was not indicated in this case.
Conclusion
Trapeziometacarpal arthrosis is a condition with a significant impact on the quality of life and it can cause worsening symptoms. Different surgical techniques are proposed such as trapeziectomy with or without ligamentoplasty or arthroplasty with implants. Our Case report described a man treated with two different techniques; it shows encouraging clinical results in favour of arthroplasty with dual mobility prosthesis. In fact, the main advantages registered and validated by the patient are the earlier return to daily activities, a better satisfaction related the restoration of the anatomical attitude of the thumb, a better range of motion and greater strength with optimal recovery even for actions that require fine movements. However, prosthetic replacement requires careful application due to a higher rate of long-term complications.
Acknowledgement
English proof reading was done by Ms. Enza Scifo.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 15, Feb 2021Accepted: Tue 02, Mar 2021
Published: Fri 19, Mar 2021
Copyright
© 2023 Saverio Comitini. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.03.11
Author Info
Saverio Comitini Giuseppe Mobilia Matteo Berti Luca Amendola Andrea Assenza Paolo Barca Marco Caponnetto Emanuela Castiello Marco Ganci Matteo Commessatti Noemi Silluzio Domenico Tigani
Corresponding Author
Saverio ComitiniDepartment of Orthopaedics and Traumatology, Ospedale Maggiore C. A. Pizzardi, Bologna, Italy
Figures & Tables
Table 1: Classification of Eaton and Littre.
|
Classification of Eaton and Littre |
|
STAGE I |
|
Normal or slightly widened trapeziometacarpal joint, normal articular contours, trapeziometacarpal subluxation |
|
STAGE II |
|
Decreased trapeziometacarpal joint space, Trapeziometacarpal subluxation, osteophytes or loose bodies less than 2 mm in diameter |
|
STAGE III |
|
Further decreased trapeziometacarpal joint space, subcohondral cysts or sclerosis, trapeziometacarpal joint of one third or more of the articular surface, osteophytes or loose bodies 2 mm or more in diameter |
|
STAGE IV |
|
Involvement of the scaphotrapezial joint or less commonly the trapeziotrapezoid or trapeziometacarpal joint to the index finger |
Table 2: Quick Dash score of right hand: Results with 12 months follow up.
|
Time |
3 months |
6 months |
12 months |
Average |
|
Open a jar |
4 |
3 |
2 |
3 |
|
Do heavy household |
3 |
2 |
2 |
2,33333333 |
|
Carrying shopping bag |
4 |
3 |
1 |
2,66666667 |
|
Wash your back |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
4 |
3 |
3 |
3,33333333 |
|
Impact recreational activities |
4 |
2 |
2 |
2,66666667 |
|
Interference with social activities |
3 |
1 |
1 |
1,66666667 |
|
Work/regular activities |
3 |
1 |
1 |
1,66666667 |
|
Pain |
2 |
1 |
1 |
1,33333333 |
|
Tingling |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
|
QDs |
43,2 |
18,2 |
11,4 |
24,2666667 |
Table 3: Quick Dash score of right hand: Results with 2 year follow up.
|
Time |
3 months |
6 months |
12 months |
2 years |
Average |
|
Open a jar |
4 |
3 |
2 |
2 |
2,75 |
|
Do heavy household |
3 |
2 |
2 |
2 |
2,25 |
|
Carrying shopping bag |
4 |
3 |
1 |
1 |
2,25 |
|
Wash your back |
1 |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
4 |
3 |
3 |
2 |
3 |
|
Impact recreational activities |
4 |
2 |
2 |
2 |
2,5 |
|
Interference with social activities |
3 |
1 |
1 |
1 |
1,5 |
|
Work/regular activities |
3 |
1 |
1 |
1 |
1,5 |
|
Pain |
2 |
1 |
1 |
1 |
1,25 |
|
Tingling |
1 |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
1 |
|
QDs |
43,2 |
18,2 |
11,4 |
9,1 |
20,475 |
Table 4: Quick Dash score: Results with 12 months follow up in arthroplasty treatment with implant.
|
Time |
3 months |
6 months |
12 months |
Average |
|
Open a jar |
3 |
2 |
1 |
2 |
|
Do heavy household |
3 |
2 |
1 |
2 |
|
Carrying shopping bag |
2 |
2 |
1 |
1,66666667 |
|
Wash your back |
1 |
1 |
1 |
1 |
|
Use of knife to cut food |
2 |
2 |
2 |
2 |
|
Impact recreational activities |
3 |
2 |
1 |
2 |
|
Interference with social activities |
3 |
2 |
1 |
2 |
|
Work/regular activities |
3 |
1 |
1 |
1,66666667 |
|
Pain |
1 |
1 |
1 |
1 |
|
Tingling |
1 |
1 |
1 |
1 |
|
Sleep |
1 |
1 |
1 |
1 |
|
QDs |
27,3 |
13,6 |
2,3 |
14,4 |
Table 5: Graded list of QuickDASH score [14, 15].
|
Interpretation |
Score |
|
Very good |
0-5 |
|
Good |
6-15 |
|
Satisfactory |
16-35 |
|
Poor |
>35 |
DASH: Disabilities of the arm, Shoulder and Hand.






References
1. Batra S, Kanvinde R (2007) Osteoarthritis of the thumb trapeziometacarpal joint. Curr Orthop 21: 135-144.
2. Sodha S, Ring D, Zurakowski D, Jupiter JB (2005) Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am 87: 2614-2618. [Crossref]
3. Wilder F V, Barrett JP, Farina EJ (2006) Joint-specific prevalence of osteoarthritis of the hand. Osteoarthr Cartil 14: 953-957. [Crossref]
4. Clifton KB, Rodner C, Wolf JM (2014) Detection of relaxin receptor in the dorsoradial ligament, synovium, and articular cartilage of the trapeziometacarpal joint. J Orthop Res 32: 1061-1067. [Crossref]
5. Choa RM, Parvizi N, Giele HP (2014) A prospective case-control study to compare the sensitivity and specificity of the grind and traction-shift (subluxation-relocation) clinical tests in osteoarthritis of the thumb carpometacarpal joint. J Hand Surg Eur Vol 39: 282-285. [Crossref]
6. Lewis S (1988) New angles on the radiographic examination of the hand--I. Radiogr Today 54: 44-45. [Crossref]
7. Ladd AL (2014) Guest editorial: The Robert’s view: A historical and clinical perspective. Clin Orthop Relat Res 472: 1097-100. [Crossref]
8. Eaton RG, Littler JW (1973) Ligament Painful Reconstruction Carpometacarpal for the Joint. J Bone Joint Surg Am 55: 1655-1666. [Crossref]
9. Bakri K, Moran SL (2015) Thumb carpometacarpal arthritis. Plast Reconstr Surg 135: 508-520. [Crossref]
10. Armstrong AL, Hunter JB, Davis TR (1994) The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Am 19: 340-341. [Crossref]
11. Henrotin Y, Raman R, Richette P, Bard H, Jerosch J et al. (2015) Consensus statement on viscosupplementation with hyaluronic acid for the management of osteoarthritis. Semin Arthritis Rheum 45: 140-149. [Crossref]
12. Trellu S, Dadoun S, Fautrel B, Gossec L (2014) AB0794 Intra-Articular Injections in Thumb Osteoarthritis. A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Rheum Dis 73.
13. Matullo KS, Ilyas A, Thoder JJ (2007) CMC arthroplasty of the thumb: A review. Hand 2: 232-239. [Crossref]
14. Phadnis J, Trompeter A, Gallagher K, Bradshaw L, Elliott DS et al. (2012) Mid-term functional outcome after the internal fixation of distal radius fractures. J Orthop Surg Res 7: 4. [Crossref]
15. Khan MS, Noordin S, Hashmi PM (2016) Intra-articular distal radius fractures: Postoperative roentgenographic and functional outcomes. J Pak Med Assoc 66: 275-279. [Crossref]
16. Brutus JP, Kinnen L (2004) Remplacement prothétique total de la trapézométacarpienne au moyen de la prothèse ARPE dans le traitement de la rhizarthrose : notre expérience à court terme dans une série personnelle de 63 cas consécutifs. Chir Main.
17. Shah DS, Middleton C, Gurdezi S, Horwitz MD, Kedgley AE (2020) The Effect of Surgical Treatments for Trapeziometacarpal Osteoarthritis on Wrist Biomechanics: A Cadaver Study. J Hand Surg Am 45: 389-398. [Crossref]
18. Davis TR, Brady O, Barton NJ, Lunn PG, Burke FD (1997) Trapeziectomy alone, with tendon interposition or with ligament reconstruction? J Hand Surg Br 22: 689-694. [Crossref]
19. Belcher HJCR, Nicholl JE (2000) A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Am 25: 350-356. [Crossref]
20. Naram A, Lyons K, Rothkopf DM, Calkins ER, Breen T et al. (2016) Increased complications in trapeziectomy with ligament reconstruction and tendon interposition compared with trapeziectomy alone. Hand (N Y) 11: 78-82. [Crossref]
21. Brennan A, Blackburn J, Thomson J, Field J (2020) Simple trapeziectomy versus trapeziectomy with flexor carpi radialis suspension: a 17-year follow-up of a randomized blind trial. J Hand Surg Eur Vol 46: 120-124. [Crossref]
22. Corain M, Zampieri N, Mugnai R, Adani R (2016) Interposition Arthroplasty Versus Hematoma and Distraction for the Treatment of Osteoarthritis of the Trapeziometacarpal Joint. J hand Surg Asian Pacific Vol 21: 85-91. [Crossref]
23. Salem H, Davis TRC (2012) Six year outcome excision of the trapezium for trapeziometacarpal joint osteoarthritis: Is it improved by ligament reconstruction and temporary Kirschner wire insertion? J Hand Surg Eur Vol 37: 211-219. [Crossref]
24. Vermeulen GM, Slijper H, Feitz R, Hovius SER, Moojen TM et al. (2011) Surgical management of primary thumb carpometacarpal osteoarthritis: A systematic review. J Hand Surg Am 36: 157-169. [Crossref]
25. Vermeulen GM, Brink SM, Slijper H, Feitz R, Moojen TM et al. (2014) Trapeziometacarpal arthrodesis or trapeziectomy with ligament reconstruction in primary trapeziometacarpal osteoarthritis: A randomized controlled trial. J Bone Joint Surg Am 96: 726-733. [Crossref]
26. Pillukat T, Mühldorfer Fodor M, Fuhrmann R, Windolf J, van Schoonhoven J (2017) Arthrodesis of the trapeziometacarpal joint. Oper Orthop Traumatol 29: 395-408. [Crossref]
