Severe and Rapid Post-Traumatic Osteolysis of the Distal Clavicle in a College Athlete: A Case Report and Review of the Literature
A B S T R A C T
Case Report: A 21-year-old female college athlete presented with continually worsening distal clavicle osteolysis. After conservative management and significant activity modification failed to resolve pain, surgical management was considered. Instability in the sagittal plane was believed to contribute to her persistent pain. Surgical management included acromioclavicular (AC) ligament reconstruction, in addition to the standard distal clavicle excision.
Conclusion: Horizontal instability in the AC joint may contribute to the failure of conservative treatment in patients with distal clavicle osteolysis. If surgical management is considered, AC ligament reconstruction, in addition to the standard distal clavicle excision, may provide additional benefit in functional outcomes.
Keywords
Post-traumatic distal clavicle osteolysis, acromioclavicular joint reconstruction, distal clavicle resection
Introduction
Distal clavicle osteolysis (DCO) is an uncommon but frequently limiting condition, especially for young, active athletes. DCO can be either traumatic or atraumatic and is believed to result from subchondral microfractures and subsequent attempts at repair [1, 2]. Typical management of DCO initially involves nonoperative options, such as physical therapy, activity modification, anti-inflammatory drugs, and intra-articular steroid injection. Surgical treatment is considered if nonoperative options are inadequate for long term pain management. The most surgical treatment for DCO is distal clavicle resection, performed either open or arthroscopic.
Superior and inferior acromioclavicular (AC) ligaments provide horizontal stability in the sagittal plane, whereas the coracoclavicular ligaments provide vertical stability of the AC joint. Renfree et al. demonstrated that resection of more than 7.6 mm of the distal clavicle in men and 5.2 mm in women might violate the superior AC ligament [3]. Horizontal stability can potentially be compromised with either pathologic or iatrogenic absence of the distal clavicle. Roedl et al. described magnetic resonance imaging (MRI) findings of 28 patients with DCO. A mean of 2.6 mm interval widening of the AC joint was noted on follow up images [4]. While horizontal instability after surgical resection of the distal clavicle has been previously reported, we are not aware of studies describing AC instability as a result of DCO [5]. We report a patient with traumatic DCO with a remarkable widening of the AC joint and subsequent horizontal instability of the AC joint that was successfully treated with distal clavicle resection and acromioclavicular ligament reconstruction.
Case Report
The patient is a 21-year-old female lacrosse player who experienced a posterior player to player hit on her right dominant shoulder while the arm was in a flexed position during a National Collegiate Athletic Association (NCAA) Division 1 women’s lacrosse game. The pain was localized over the AC joint and was worse with overhead and cross-body activities. Physical examination revealed tenderness over the AC joint, discomfort with cross-body adduction, and pain with O’Brien test. The range of motion was limited by pain to 120○ of flexion and 120○ of abduction. Initial radiographs were negative for significant abnormality (Figure 1), and a diagnosis of AC joint sprain was made. The patient was treated with ice and physical therapy, in addition to a supportive brace while playing lacrosse. She continued competing for an additional month, until the conclusion of her season. Following the conclusion of the competitive season, she took a full month off from any activity; the pain was better but still occasionally present.
Figure 1: Radiographs after the initial trauma were unremarkable.
Three months after the initial injury, in preparation for the following season, the patient resumed lifting and running training and began experiencing worsening pain with activity and at rest. MRI showed bone marrow edema denoting erosive changes along the distal clavicle related to post-traumatic osteolysis (Figure 2). Weightlifting activity was minimally modified, and two steroid injections were provided 3 months apart to get her through the season. The injections improved her pain only partially and temporarily.
Figure 2: A & B) T2 coronal MRI cuts 3 months after initial injury showing hyperintense signal denoting erosive changes and distal clavicle osteolysis.
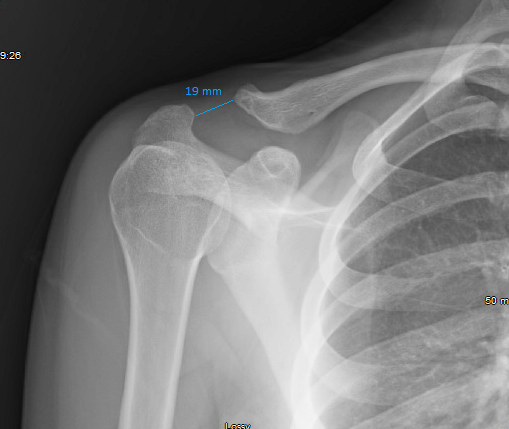
One year after the initial injury, her pain was persistent with similar physical examination findings. Radiographs showed progressive osteolysis (Figure 3). Following the completion of her senior lacrosse season, the patient significantly modified activity, which included no running, lifting, or shoulder weight bearing exercises for three months. Activity modification provided little to no pain relief. Radiographs 18 months after the initial injury revealed further widening of the AC joint measuring 19 mm (Figure 4). At that time, the decision was made to proceed with surgical treatment. Horizontal AC instability in the sagittal plane was believed to contribute to her persistent symptoms, so both the bony pathology and the joint stability were addressed.
Figure 3: Radiograph 1 year after initial injury showing progressive osteolysis and tapering of the distal clavicle.
Figure 4: Radiograph 18 months after initial injury showing progressive osteolysis and tapering of the distal clavicle. Note the wide gap of the AC joint compared to preoperative radiograph which was measured to be 19 mm.
Surgical Technique
After adequate general anesthesia, the patient was placed in the beach-chair position. The right shoulder was prepped and draped. A superior approach was utilized to dissect down to the clavicle. Remarkable horizontal instability was noted on examination intraoperatively. The distal end of the clavicle was debrided and reamed down the clavicular shaft to stimulate biologic healing. A 5 mm reamer was drilled from anterior to posterior in the metaphyseal region over a guide pin. On the acromial end, two blind-ended tunnels were made. A semitendinosus allograft was passed through the clavicular tunnel; then the two ends were passed through the acromial tunnels and fixed using the docking technique as described by Kibler et al. [6]. Good horizontal stability was achieved. The patient was kept in a sling for 4 weeks while maintaining a passive range of motion. Active assisted and strengthening exercises were gradually started after 6 weeks.
The patient’s symptoms progressively improved during the first few months after surgery. At 6 months post-operation, she had no pain at rest and mild pain with running and physical activities. She continued to improve afterwards, and at 12 months post-operation, she had minimal discomfort only with certain activities. Her range of motion was full in all planes. The AC joint was stable in the anteroposterior direction on examination. American Shoulder and Elbow Surgeons (ASES) Standardized Shoulder Assessment, Simple Shoulder Test (SST), and Single Assessment Numeric Evaluation (SANE) were completed pre-operatively, as well as 6 months and 12 months post-operatively, and showed gradual progressive improvement in all scores (Table 1).
Table 1: Preoperative and postoperative functional parameters.
|
|
Preoperative |
6 months |
12 months |
|
ASES |
57 |
78 |
85 |
|
SST |
83% |
92% |
100% |
|
SANE |
50% |
75% |
95% |
Discussion
Distal clavicle osteolysis is an uncommon shoulder pathology that is most commonly reported in male weightlifters [7]. The patient described in this report is a female lacrosse player with a greater amount of distal clavicle recession, leading to a significantly wider area of osteolysis compared to previous comparable reports. This patient’s case is unique for two reasons: 1) the extent to which her distal clavicle receded, and 2) her persistent and unchanged pain frequency and intensity following a prolonged period of nonoperative management.
In a series of 28 patients with DCO who underwent MRIs at least 2 years apart, the mean AC joint width increased from 2.4 mm to 5 mm (2.6 mm interval widening) [4]. The authors noted that a healthy AC joint is considered to have a width of less than 6 mm [4]. In the patient described in this report, the AC joint width increased from 5.4 mm to 19 mm over a period of 18 months. The remarkable interval widening, and her unresolved pain led us to believe that instability in the sagittal plane was the source of her pain. This instability was addressed with AC ligament reconstruction. While this study only discusses one patient, her significant pain resolution strongly suggests that DCO patients failing to improve with conservative treatment may have horizontal AC joint instability and can potentially benefit from AC ligament reconstruction.
AC ligament reconstruction procedures are traditionally only used in surgical treatment of high-grade AC joint separations (grades III-VI), as outlined by the Rockwood classification [8]. Apart from high-grade traumatic AC joint separations, instability in the AC joint resulting from excessive anterior-posterior motion has been theorized as a potential source of shoulder pain [9]. Blazar et al. demonstrated that the amount of anterior-posterior movement after surgical resection of the distal clavicle directly correlated with the amount of postoperative pain [5].
While the significantly increased AC joint space in this patient, led to the proposed excessive joint instability and pain, AC joint stability is seldom addressed during distal clavicle excision. AC joint instability in the anterior-posterior direction in patients with DCO should be considered, particularly if bone resorption exceeds 5 mm. If AC joint instability is present, this could be a potential source of long-term pain. Additionally, AC joint instability after distal clavicle resection can be expected. Persistent pain after distal clavicle resection for DCO secondary to horizontal AC instability may warrant consideration amongst shoulder specialists of adding AC joint reconstruction to standard treatment. Evaluation of AC joint stability in the setting of DCO should be investigated further in future studies.
Conflicts of Interest
None.
Consent
The patient was informed that data concerning her injury and treatment would be submitted for publication, she consented.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 18, May 2020Accepted: Wed 03, Jun 2020
Published: Fri 12, Jun 2020
Copyright
© 2023 Katharine Schuyler Nissen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.09
Author Info
Brian M. Grawe Katharine Schuyler Nissen Yehia H. Bedeir
Corresponding Author
Katharine Schuyler NissenUniversity of Pennsylvania, Perelman Center for Advanced Medicine, Philadelphia, Pennsylvania, USA
Figures & Tables
Table 1: Preoperative and postoperative functional parameters.
|
|
Preoperative |
6 months |
12 months |
|
ASES |
57 |
78 |
85 |
|
SST |
83% |
92% |
100% |
|
SANE |
50% |
75% |
95% |



References
- Cahill BR (1982) Osteolysis of the Distal Part of the Clavicle in Male Athletes. J Bone Joint Surg Am 64: 1053-1058. [Crossref]
- Brunet ME, Reynolds MC, Cook SD, Brown TW (1986) Atraumatic Osteolysis of the Distal Clavicle: Histologic Evidence of Synovial Pathogenesis. A Case Report. Orthopedics 9: 557-559. [Crossref]
- Renfree KJ, Riley MK, Wheeler D, Hentz JG, Wright TW (2003) Ligamentous Anatomy of the Distal Clavicle. J Shoulder Elbow Surg 12: 355-359. [Crossref]
- Roedl JB, Nevalainen M, Gonzalez FM, Dodson CC, Morrison WB et al. (2015) Frequency, Imaging Findings, Risk Factors, and Long-Term Sequelae of Distal Clavicular Osteolysis in Young Patients. Skeletal Radiol 44: 659-666. [Crossref]
- Blazar P, Iannotti JP, Williams GR (1998) Anteroposterior Instability of the Distal Clavicle After Distal Clavicle Resection. Clin Orthop Relat Res 348: 114-120. [Crossref]
- Kibler WB, Sciascia AD, Morris BJ, Dome DC (2017) Treatment of Symptomatic Acromioclavicular Joint Instability by a Docking Technique: Clinical Indications, Surgical Technique, and Outcomes. Arthroscopy 33: 696.e2-708.e2. [Crossref]
- Schwarzkopf R, Ishak C, Elman M, Gelber J, Strauss DN et al. (2008) Distal Clavicular Osteolysis: A Review of the Literature. Bull NYU Hosp Jt Dis 66: 94-101. [Crossref]
- Rockwood Jr C (1984) Injuries to the acromioclavicular joint: Subluxations and dislocations about the shoulder. Fract Adults Philadelphia: JB Lippincott 860-910.
- Flatow EL (1993) The Biomechanics of the Acromioclavicular, Sternoclavicular, and Scapulothoracic Joints. Instr Course Lect 42: 237-245. [Crossref]
