Simulation Using Augmented Reality to Teach Body Angle Positioning for Radiography
A B S T R A C T
When students learn radiographic positioning during radiography practical training in educational institutions, they adjust the angle of the body using positioning aids and angle gauges. In contrast, radiologic technologists position patients using their own hands in clinical environments. In recent years, virtual simulations have been used to help students improve their clinical skills. However, because the existing simulations use computer-generated virtual environments, students cannot actually position human bodies or anthropomorphic phantoms. Therefore, we developed a simulation using augmented reality to teach radiographic positioning. This simulation allows learners to simulate angle placement by using both hands without positioning aids and angle gauges by looking at a virtual object that demonstrates the angle. The objective of this study was to investigate whether this simulation can be applied as a learning tool for radiography practical training and to examine future development directions for this simulation. We introduced the simulation in radiography practical training. The lumbar spine oblique projection was chosen as a learning task in this study, and an anthropomorphic phantom was used for practice. A questionnaire survey was conducted to collect feedback from the students at the end of the semester (n = 41). The survey results indicated that the students could practice positioning the angle of the body using only their own hands, demonstrating that the simulation could be applied as a learning tool in radiography practical training. Ongoing work will be conducted to develop a simulation in which students can practice with a human body.
Keywords
Radiography, practical training, augmented reality
Introduction
Patient positioning strongly influences the accuracy of acquired diagnostic information and is a difficult skill to master [1]. In general, when students learn radiographic positioning during radiography practical training in educational institutions, body angle positioning is practiced on anthropomorphic phantoms or fellow students using positioning aids and angle gauges. However, because radiologic technologists in clinical environments must obtain radiographs quickly to reduce the burden on the patient and maintain the workflow in the hospital, they position patients appropriately using their hands. To become able to adjust the angle of the body without relying on positioning aids and angle gauges, it is essential to practice positioning techniques using both hands. Hence, a learning method that more closely imitates the process performed in clinical environments and that enables students to use their own hands is required.
In recent years, virtual simulations have been used to help students improve their clinical skills in radiography education [2-8]. These simulations provide training for tasks such as radiographic positioning, image evaluation, radiographic equipment arrangement, and radiographic procedures. However, because the existing simulations use computer-generated virtual environments for learning, students cannot actually position human bodies or anthropomorphic phantoms.
Therefore, we developed a simulation using augmented reality (AR) to teach students how to position a body for radiography. AR technology displays virtual objects in a real environment [9]. By using AR, learners can practice while being supported by virtual objects in a real environment rather than in a virtual environment [9-11]. Our simulation allows learners to simulate angle placement by using both hands without positioning aids and angle gauges. Instead, they look at a virtual object that demonstrates the angle. The aim of this study was to investigate whether the simulation can be applied as a learning tool in radiography practical training and to examine the direction of future development of this simulation.
Materials and Methods
I Ethical Approval
Ethical approval for this study was obtained from the Tokyo Metropolitan University Arakawa Campus Research Safety Ethics Committee (approval number 18016). Informed consent was obtained from all participants, and the anonymity of the survey results was ensured.
II System Configuration
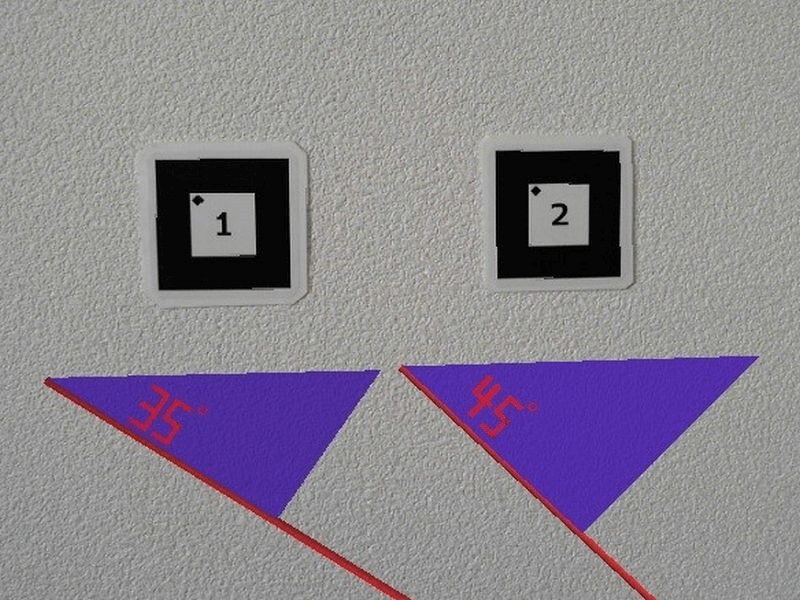
The simulation displays a triangular virtual object on a camera image by detecting a fiducial marker using the web camera of a notebook computer (Figure 1). The virtual object can be moved to any position clicked on the camera image. A STYLE-15FX061-i7-KS notebook computer (Iiyama, Kanagawa, Japan), running Windows 10 (64 bit) and equipped with a GeForce MX150 GPU, 15.6-inch (1920×1080) display, and 4166 MB video RAM, was used. A LifeCam Studio camera (Microsoft Corporation, Washington, USA) was employed as the web camera.
Figure 1: Fiducial markers and virtual objects used in the study.
Metasequoia 4.6 (ver. 4.6.4) for Windows (Tetraface Inc., Tokyo, Japan) was used to create the virtual objects. Metasequoia is a type of three-dimensional modeling software for creating and editing three-dimensional data. ARToolKit was used to implement the technology in the simulation [12]. ARToolKit estimates the position and pose of the fiducial marker accurately and displays the virtual object in real time. ARToolKit can also create the fiducial marker; we created a 60 × 60 mm marker with this function.
III Learning Task
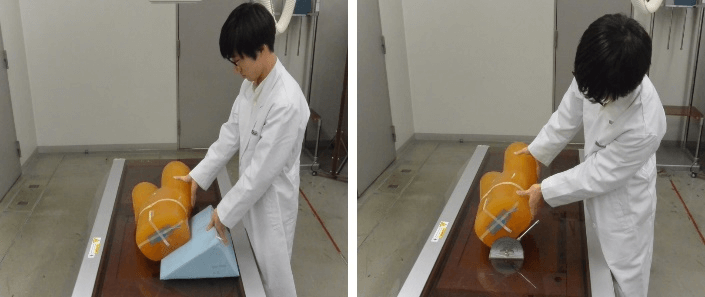
Positioning of the lumbar spine oblique projection (at 35° and 45°) was chosen as the learning task in this study. When performing this projection, technologists use both hands to adjust the angle of the waist of a patient lying on the radiographic table. In educational institutions, students learn this technique using positioning aids and angle gauges. However, positioning aids make one hand unusable, and angle gauges are not suitable for repeating practice while confirming the current angle because the scale is far from the eye of the learner (Figure 2).
Figure 2: Examples of learning using a positioning aid (left) and an angle gauge (right).
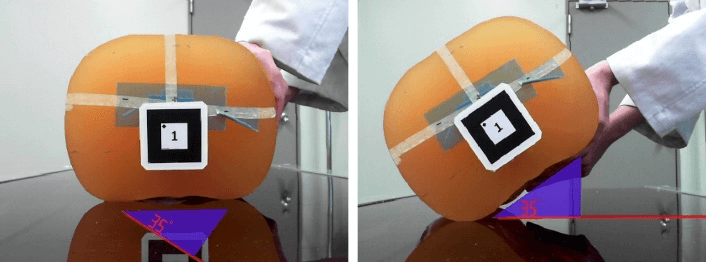
Figure 3: Example of learning using the simulation.
Figure 4: Before positioning (left) and after positioning (right).
In contrast, by using the simulation, learners can repeatedly practice positioning the angle of the body with both hands while checking whether the angle is excessive or insufficient. Although the simulation requires the positioning angle and camera image size to be selected for setup, learners only look at the virtual object during practice. Figure 3 shows a learner positioning an anthropomorphic phantom using the simulation. Body angle positioning is achieved by lifting the anthropomorphic phantom so that the line extending from the triangle is horizontal on the camera image (Figure 4). The learner uses the following methods.
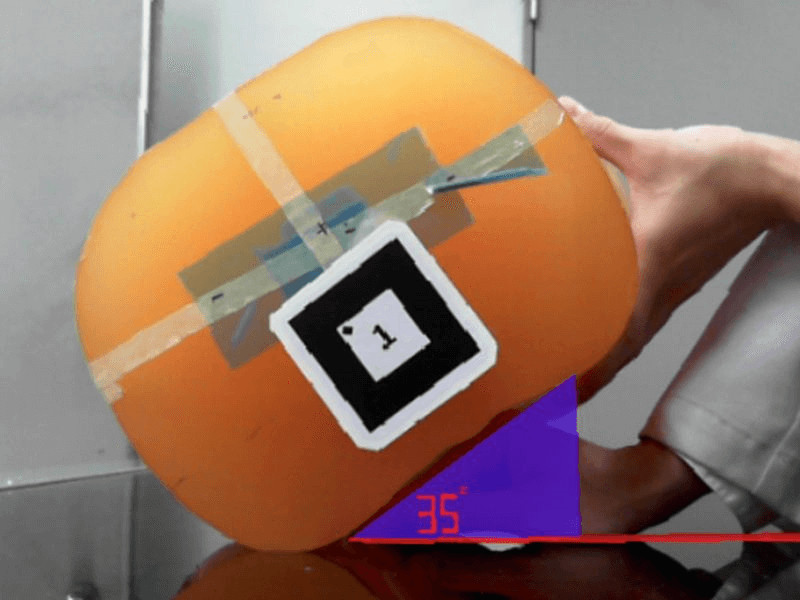
i. The learner repeatedly positions the angle of the anthropomorphic phantom with both hands while observing the virtual object. Next, he or she adjusts the angle without looking at the virtual object.
ii. The learner puts his or her hand on the back of the anthropomorphic phantom and remembers the angle in the form of the hand (Figure 5). Next, he or she adjusts the angle using the hand as an angle gauge without looking at the virtual object.
Figure 5: Example of learning via the simulation.
IV Participants
We introduced the simulation to a unit of lumbar spine radiography in radiography practical training in 2018. Forty-one third-year students in the Department of Radiological Sciences at Tokyo Metropolitan University participated in the class. The students who attended the training were taught anatomy, image evaluation, and the theory of radiographic positioning protocols in didactic lectures by their second year. We verbally explained the learning methods using the simulation just before it was employed during class. Students practiced how to adjust the angle of the body for the oblique projection with the anthropomorphic phantom using the simulation as well as positioning aids and angle gauges.
V Student Feedback Collection and Analysis
A questionnaire survey was conducted to investigate whether the simulation could be applied as a learning tool in radiography practical training at the end of the semester. The survey questions were scored using a five-point Likert-scale, and an open-ended question regarding learning using the simulation was included. However, because the simulation involves computer technology, students who perceived their computer technology abilities to be lower could have been less satisfied with the learning process than students who perceived their abilities to be higher [2]. Hence, to assess whether the training was provided equally, we included a four-point Likert-scale question regarding the perception of the students of their confidence using computer technology, referring to a study by Shanahan [2]. The chi-squared test was used to analyse whether there was a difference in the computer confidence levels of the students. The polychoric correlation coefficient was used to analyse whether there was a correlation between the computer confidence levels of the students and their responses to the questions regarding learning using the simulation. The survey data were entered into R3.6.0; the significance threshold was p < 0.05.
Results
Responses were received from 41 students (response rate 100%), including 23 females and 18 males ranging in age from 20 to 22 years. All students had no prior experience of using the simulation. The distribution of responses to the question regarding the perceptions of the students of their confidence using computer technology is presented in (Table 1). The responses “not confident” and “not very confident” accounted for 70.7% (χ2 = 7.05, p = 0.008) of the total. The distribution of responses to the questions regarding learning using the simulation is presented in (Table 2).
Table 1: Student perceptions of confidence using computer technology (n = 41).
|
Question (Likert scale) |
Confident |
Moderately confident |
Not very confident |
Not confident |
|
Please tell us your confidence using computer technology |
0 (0%) |
12 (29.3%) |
26 (63.4%) |
3 (7.3%) |
Table 2: Responses to the questions regarding learning using the simulation (n = 41).
|
Questions 1–6 (Likert scale) |
SA |
A |
N |
D |
SD |
|
1: It was effective for improving the skill of positioning the body angle |
19 (46.3%) |
22 (53.7%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
2: It was effective for improving confidence in the skill of positioning the body angle |
3 (7.3%) |
24 (58.5%) |
12 (29.3%) |
2 (4.9%) |
0 (0%) |
|
3: It was more effective than using positioning aids and angle gauges |
17 (41.5%) |
24 (58.5%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
4: It was easy to use |
30 (73.2%) |
11 (26.8%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
5: It was useful as a learning tool |
21 (51.2%) |
20 (48.8%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
6: Actively incorporating it into the classes will improve the quality of the class |
18 (43.9%) |
23 (56.1%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
Question 7 (free answer) |
|||||
|
7: Please tell us what you thought about learning using the simulation |
|||||
|
It was easy to use and understand the angles. (one person) |
|||||
|
It was better to be able to repeat adjusting the angle quickly than to use positioning aids and angle gauges. (one person) |
|||||
|
I would like to try with a human body. (two persons) |
|||||
SA: Strongly Agree; A: Agree; N: Neither agree nor disagree; D: Disagree; SD: Strongly Disagree.
All of the students responded positively to question 1 and questions 3-6. Although there were some “neither agree nor disagree” (n = 12, 29.3%) or “disagree” (n = 2, 4.9%) responses for question 2, most of the responses to the questions regarding learning using the simulation were positive. There was no significant correlation between the responses to question 2 and the computer confidence levels of the students (ρ = −0.03, p = 0.13).
Discussion
For the question regarding the perception of the students of their confidence using computer technology, most students responded with “not confident” and “not very confident.” However, the students highly valued the learning using the simulation regardless of their confidence levels, which is certainly because they were able to concentrate on the learning task as they did not need to operate the PC during practice. Consequently, it can be inferred that even students who perceived that they were not good at using computer technology practiced with no difficulty. Therefore, the study results indicate that the students could practice positioning the angle of the body using their own hands without positioning aids and angle gauges, demonstrating that the simulation could be applied as a learning tool in radiography practical training.
Radiographic positioning is very difficult to master, and considerable practical experience is required to improve this skill. In a digital radiography system, the main cause of image rejection/retaking in clinical environments has been revealed to be positioning errors [13-17]. Nol et al. reported that positioning errors are largely associated with less experienced technologists and are mainly due to the rotation of body parts [17]. While it is necessary to plan education and training for technologists in clinical facilities, educational institutions should also allow students to experience radiographic positioning in a manner close to that in clinical practice to improve their skills [13-17].
In this study, by using virtual objects instead of positioning aids and angle gauges, a new teaching method for radiographic positioning techniques that imitated clinical practice and enabled students to use both hands to adjust the angle of the body was proposed. Although we dealt with only one projection method, the simulation was successfully introduced into radiography practical training. Following the results, plans are being made to use this simulation for other body parts.
The novelty of our simulation for virtual simulations using virtual patients is that students can actually experience positioning techniques. Because the existing simulations use a mouse, keyboard, or touch-screen system for learning, students cannot position human bodies or anthropomorphic phantoms. Thus, the results suggest that AR is a potentially useful teaching technology that should be developed further for education related to radiographic positioning.
However, simulated learning environments cannot completely reproduce situations that occur in clinical environments [18]. The simulation was used to teach basic positioning techniques in this training. Meanwhile, the teacher instructed the students regarding how to communicate with the patient and the amount of force used to manipulate a patient who is in pain or has limited movement. Hence, it should be noted that the simulation does not cover every aspect of teaching radiographic positioning.
In addition, the simulation uses not a human body, but rather an anthropomorphic phantom for practice. Technologists must pay attention not only to the angle of the imaging site, but also to the twisting of the joints when positioning the patient. However, the simulation only allows students to adjust the angle of the imaging site. We believe that this characteristic may have affected the responses to the following two questions in the survey results. First, there were some “neither agree nor disagree” or “disagree” responses to the statement, “It was effective for improving confidence in the skill of positioning the body angle.” Second, two students commented that they would like to try with a human body when asked for their impressions of the learning methods using the simulation. Accordingly, we are currently developing a more practical simulation that can provide students with an environment in which they can practice positioning the angle of a human body.
Limitations
The students who participated in the study had no experience in clinical training, and student perceptions of the learning process may vary with their clinical experience. This study assessed whether the developed simulation can be applied as a learning tool for radiography practical training. However, its effectiveness was not validated. In a future study, feedback should be collected from students who have clinical training experience and the learning effects of the simulation should be measured quantitatively.
Conclusion
The results of this study indicate that the developed simulation could be applied as a learning tool in radiography practical training. This study has the following two implications. First, a new teaching method was proposed for radiographic positioning that imitates clinical practice and enables students to use both hands to adjust the angle of the body. Second, the results suggest that AR is a potentially useful teaching technology that should be developed further for education related to radiographic positioning. We are currently designing a more practical simulation in which students can practice positioning the angle of a human body.
Acknowledgements
The authors wish to acknowledge Professor Atsushi Senoo, who is in charge of radiography practical training at the Tokyo Metropolitan University, for allowing the use of the simulation in radiography practical training. The authors also wish to thank and acknowledge Mr. Ken Gonoi, Graduate School of Political Science, Waseda University for his helpful advice on the writing structure.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 24, Jul 2020Accepted: Thu 06, Aug 2020
Published: Fri 14, Aug 2020
Copyright
© 2023 Shin Nagamata. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2020.03.03
Author Info
Corresponding Author
Shin NagamataDepartment of Radiological Sciences, Graduate School of Human Health Sciences, Tokyo Metropolitan University, Tokyo, Japan
Figures & Tables
Table 1: Student perceptions of confidence using computer technology (n = 41).
|
Question (Likert scale) |
Confident |
Moderately confident |
Not very confident |
Not confident |
|
Please tell us your confidence using computer technology |
0 (0%) |
12 (29.3%) |
26 (63.4%) |
3 (7.3%) |
Table 2: Responses to the questions regarding learning using the simulation (n = 41).
|
Questions 1–6 (Likert scale) |
SA |
A |
N |
D |
SD |
|
1: It was effective for improving the skill of positioning the body angle |
19 (46.3%) |
22 (53.7%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
2: It was effective for improving confidence in the skill of positioning the body angle |
3 (7.3%) |
24 (58.5%) |
12 (29.3%) |
2 (4.9%) |
0 (0%) |
|
3: It was more effective than using positioning aids and angle gauges |
17 (41.5%) |
24 (58.5%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
4: It was easy to use |
30 (73.2%) |
11 (26.8%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
5: It was useful as a learning tool |
21 (51.2%) |
20 (48.8%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
6: Actively incorporating it into the classes will improve the quality of the class |
18 (43.9%) |
23 (56.1%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
Question 7 (free answer) |
|||||
|
7: Please tell us what you thought about learning using the simulation |
|||||
|
It was easy to use and understand the angles. (one person) |
|||||
|
It was better to be able to repeat adjusting the angle quickly than to use positioning aids and angle gauges. (one person) |
|||||
|
I would like to try with a human body. (two persons) |
|||||
SA: Strongly Agree; A: Agree; N: Neither agree nor disagree; D: Disagree; SD: Strongly Disagree.

References
- Lampignano J, Kendrick LE (2017) Workbook for Bontrager's Textbook of Radiographic Positioning and Related Anatomy - E-Book. 9th Edition. Elsevier Health Sciences. St. Louis, MO.
- Shanahan M (2016) Student perspective on using a virtual radiography simulation. Radiography 22: 217-222.
- Sapkaroski D, Baird M, McInerney J, Dimmock MR (2018) The implementation of a haptic feedback virtual reality simulation clinic with dynamic patient interaction and communication for medical imaging students. J Med Radiat Sci 65: 218-225. [Crossref]
- Sapkaroski D, Baird M, Mundy M, Dimmock MR (2019) Quantification of student radiographic patient positioning using an immersive virtual reality simulation. Simul Healthc 14: 258-263. [Crossref]
- Sapkaroski D, Mundy M, Dimmock MR (2020) Virtual reality versus conventional clinical role-play for radiographic positioning training: A students' perception study. Radiography 26: 57-62. [Crossref]
- Bridge P, Gunn T, Kastanis L, Pack D, Rowntree P et al. (2014) The development and evaluation of a medical imaging training immersive environment. J Med Radiat Sci 61: 159-165. [Crossref]
- Ahlqvist JB, Nilsson TA, Hedman LR, Desser TS, Dev P et al. (2013) A randomized controlled trial on 2 simulation-based training methods in radiology: Effects on radiologic technology student skill in assessing image quality. Simul Healthc 8: 382-387. [Crossref]
- Gunn T, Jones L, Bridge P, Rowntree P, Nissen L et al. (2018) The use of virtual reality simulation to improve technical skill in the undergraduate medical imaging student. Interact Learn Environ 26: 613-620.
- Azuma RT (1997) A survey of augmented reality. Presence Teleoperators Virtual Environ 6: 355-385.
- Chen YH, Wang CH (2018) Learner presence, perception, and learning achievements in augmented-reality-mediated learning environments. Interact Learn Environ 26: 695-708.
- Tang A, Biocca F, Lim L (2004) Comparing differences in presence during social interaction in augmented reality versus virtual reality environments: An exploratory study. Presence Teleoperators Virtual Environ 204-207.
- Kato H, Billinghurst M (1999) Marker tracking and HMD calibration for a video-based augmented reality conferencing system. Proc 2nd IEEE ACM Int Workshop Augment Real (IWAR’99), San Francisco, USA 85-94.
- Atkinson S, Neep M, Starkey D (2020) Reject rate analysis in digital radiography: an Australian emergency imaging department case study. J Med Radiat Sci 67: 72-79. [Crossref]
- Hofmann B, Rosanowsky TB, Jensen C, Wah KH (2015) Image rejects in general direct digital radiography. Acta Radiol Open 4: 1-6. [Crossref]
- Waaler D, Hofmann B (2010) Image rejects/retakes--radiographic challenges. Radiat Prot Dosimetry 139: 375-379. [Crossref]
- Nol J, Isouard G, Mirecki J (2006) Digital repeat analysis; setup and operation. J Digit Imaging 19: 159-166. [Crossref]
- Nol J, Isouard G, Mirecki J (2005) Uncovering the causes of unnecessary repeated medical imaging examinations, or part of, in two hospital departments. Radiographer 52: 26-31.
- Liley T, Ryan E, Lee K, Dimmock M, Robinson J et al. (2018) Student perceptions of remote access simulated learning in computed tomography. Interact Learn Environ. https://doi.org/10.1080/10494820.2018.1546746
