Soft Tissue Tumor Leg - A Rare Presentation of Cutaneous Rhinosporidiosis
A B S T R A C T
Rhinosporidiosis presents commonly as polypoidal growth in nose, but presentation in other sites including skin, genitourinary tract is documented. Cutaneous presentation is rare, which may present as pedunculated swelling or cutaneous ulceration, but presenting as soft tissue tumor is extremely rare. The multifaceted presentation of the disease causes diagnostic dilemma to an unsuspecting physician. Clinical and radiological findings may mislead, but usually typical history helps, and typical histology clinches the diagnosis. We are presenting a case of disseminated cutaneous rhinosporidiosis presented as soft tissue mass lesion in the leg causing diagnostic difficulty due to the rare presentation.
Keywords
Rhinosporidiosis, cutaneous presentation, tumor
Introduction
Rhinosporidiosis is a primary disease of nasopharyngeal domain, although primary and secondary dissemination to other parts of body are reported [1]. Cutaneous lesions are rare in occurrence, usually caused by hematogenous dissemination. Both hematogenous and lymphatic spread could cause generalized cutaneous lesions, while direct inoculation results in the primary type [2]. The multifaceted presentation of cutaneous rhinosporidiosis includes sessile polyps, subcutaneous nodules, cutaneous horn, verruca vulgaris look alike, and ulcerated lesions, causing diagnostic dilemma to the unsuspecting physician [3, 4]. This case is presented to highlight the rare presentation as tumor.
Case Report
A 58-year-old male from southern part of India, a known case of recurrent nasopharyngeal rhinosporidiosis, presented with a painless swelling in the left leg of two weeks duration. On examination, a subcutaneous swelling of size 2x1.5cm was seen with no associated findings. As the patients was recently diagnosed as a case of early myelofibrosis with persistent low platelet levels and with the history of aspirin intake, localized hematoma of calf muscle was suspected. He was advised to undergo local sonography but lost to follow-up. He reported back after two months, with rapid increase in size. On examination, the swelling was about 15x8cm size (Figure 1), hard, non-tender, non-compressible, skin over the swelling stretched and shiny, visible veins over the swelling and absence of any local or regional inflammatory signs. Other systemic examinations were negative. With the history of rapid growth and absence of corroborating clinical evidence of inflammation, tumor pathology was suspected. Ultra-sonogram of left leg suggested soft tissue lesion.
Figure 1: Tumor of left leg.
Figure 2: MRI showing heterogenous lesion of size 10.6x9.3cm.
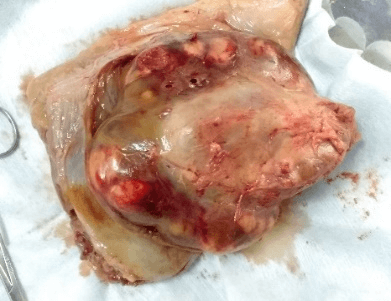
Figure 3: Excised specimen.
MRI showed heterogeneous lesion of size 10.6x9.3cm with faint septations and suggested possibility of sarcoma (Figure 2). Trucut biopsy was done to assess the pathology, which revealed characteristic sporangia in various stages of maturation, clinching the diagnosis. Our patient had previous episodes of nasal and laryngeal involvement but at the present presentation, no lesions in the nasopharynx or in the visceral organs like lungs, liver, kidney or retroperitoneum were detected. The presenting leg lesion was surgically excised in-toto along (Figure 3), with its deep fascial attachments and primary skin closure was done. Postoperative period was uneventful, and patient is symptom free till now, 3 years and 6 months after surgery.
Discussion
Cutaneous rhinosporidiosis, although known, is very rare [5]. Hematologic spread is considered as a main reason for distant spreads [6]. It causes diagnostic dilemma, with varied modes of presentation. Usually it presents to dermatologist with subcutaneous nodules, plaques, sessile polyps or ulcerated lesions, but presentation as tumor is very rare. ‘Rhinosporidioma’ is the name given for tumoral cutaneous rhinosporidiosis, by Date et al. [7]. Literature documentation of such ‘rhinosporidioma’ is very rare. One more interesting factor noticed in Indian patients is that patients with blood group ‘O’ has the highest incidence of 70% [8]. The blood group of our patient (ABO blood group: ‘O’) confirms that finding. Wide excision with electrocoagulation of the lesion base is the preferred method of management. Although cases of spontaneous regression have been recorded, they are few and rare, to warrant regular use. Dapsone may be tried as an adjuvant to surgical management. Our case was clinically and radiologically suspected as a soft tissue tumor. It was a diagnostic challenge for the physician, but for cytological diagnosis. This case asserts the clinician to be suspicious of all cutaneous lesions, in patients with rhinosporidiosis, because the diverse clinical presentation may faze the physician.
Funding
None.
Source of Support
None.
Conflicts of Interest
None.
Consent
Informed Consent was obtained from the patient.
Article Info
Article Type
Case ReportPublication history
Received: Mon 20, Apr 2020Accepted: Thu 30, Apr 2020
Published: Wed 06, May 2020
Copyright
© 2023 R. Chithra. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.02.08
Author Info
B Sai Dhandapani R King Gandhi R. Chithra
Corresponding Author
R. ChithraDepartment of General Surgery, Southern Railway Head Quarters Hospital, Ayanavarum, Chennai, India
Figures & Tables


References
- Kumari R, Laxmisha C, Thappa DM (2005) Disseminated cutaneous rhinosporidiosis. Dermatol Online J 11: 19. [Crossref]
- Arseculeratne SN (2002) Recent advances in rhinosporidiosis and Rhinosporidium seeberi. Indian J Med Microbiol 20: 119-131. [Crossref]
- Thappa DM, Venkatesan S, Sirka CS, Jaisankar TJ, Gopalkrishnan et al. (1998) Disseminated cutaneous rhinosporidiosis. J Dermatol 25: 527-532. [Crossref]
- Nayak S, Acharjya B, Devi B, Sahoo A, Singh N (2007) Disseminated cutaneous rhinosporidiosis. Indian J Dermatol Venereol Leprol 73: 185-187. [Crossref]
- Shenoy MM, Girisha BS, Bhandari SK, Peter R (2007) Cutaneous rhinosporidiosis. Indian J Dermatol Venerol Leprol 73: 179-181. [Crossref]
- Rajam RV, Viswanathan GC (1955) Rhinosporidiosis: A study with a report of a fatal case with systemic dissemination. Ind J Surg 17: 269-298.
- Date A, Ramkrishna B, Lee VN, Sundraraj GD (1995) Tumoral rhinosporidiosis. Hiatopathology 27: 288-290. [Crossref]
- Kameswaran S, Lakshmanan M (1999) Rhinosporidiosis. In: Kameswaran S, Kameswaran M, editors. ENT disorders in a tropical environment. Chennai: MERF Publications 19.
