Spinal Cord Compression Due to Hypertrophic Dorsal Pachymeningitis in a Patient with ANCA + Vasculitis
A B S T R A C T
Hypertrophic pachymeningitis is an infrequent cause of spinal cord compression, secondary to an intracanal and extramedullary inflammatory infiltrate in patients with Wegener’s disease, and it produces canal stenosis and spinal cord compression. We present the case of a patient with this rare entity, providing explanatory images, who was treated with corticosteroids with partial remission of the lesions.
Keywords
Wegener’s disease, spinal cord compression, MRI
Case Report
We present the case of a 72-year-old male patient with a long-standing history of ANCA + vasculitis, suggestive of Wegener's granulomatosis, who came to the emergency room due to progressive weakness and a sensation of corking in the left lower limb, of acute onset.
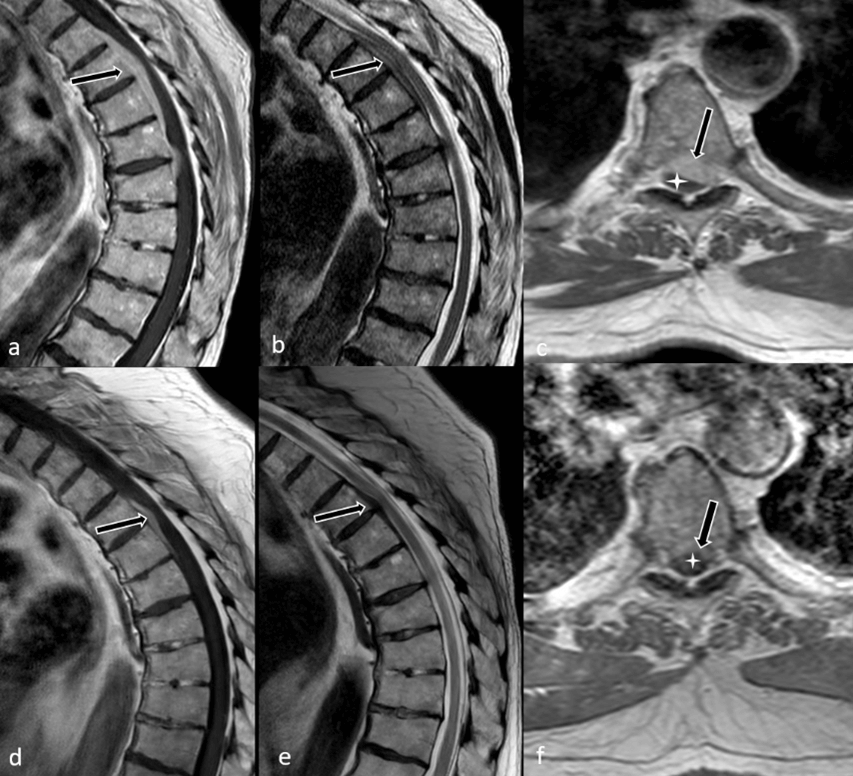
In the anamnesis, he referred right rib pain in the days before, and in the three days before the request for assistance, sphincter dysfunction. In the clinical examination, a right D8 sensory level was also detected. An urgent dorsal spine MRI was performed, which showed a solid intracanal and extramedullary lesion extending from D4 to D8 (Figures 1a-1c, black arrow with white border), which seemed to depend on the dura mater, predominantly occupying the anterior quadrants of the canal [1]. On imaging, it was a hypointense T2 lesion (Figure 1b), and it experienced avid uptake of intravenous contrast (Figures 1a & 1c). It was composed of several nodulations that conditioned spinal canal stenosis (Figure 1c, white cross) and compression of the dorsal cord, although no evidence of myelopathy at the time of the examination was seen [2].
Given the suspicion of inflammatory pachymeningitis, it was decided to undergo treatment by means of intravenous cyclophosphamide cycles, associated with rituximab and prednisone, as well as rehabilitation in a spinal cord injury unit [3]. After 6 months of treatment, the patient experienced an evident improvement in gait, as well as in pain, and the control MRI (Figures 1d-1f) showed a decrease in the volume of the lesion as well as a lesser degree of cord compression.
Figure 1: Dorsal spine MRI pre (a, b, c) and post treatment (d, e, f). Sagittal T1-TSE post gadolinium (a, d), Sagittal T2-TSE (b, e) and Axial T1-TSE post gadolinium (c, f). A solid intracanal and extramedullary lesion extending from D4 to D8 is seen (black arrow with white border), conditioning spinal canal stenosis (white cross).
Conclusion
Hypertrophic pachymeningitis is an infrequent cause of spinal cord compression that can be managed conservatively with adequate magnetic resonance imaging, and that can respond to corticosteroid therapy, without the need for decompressive surgery.
Author Contributions
Conception and design of the manuscript: JPMB, MRP, PPN; Data collection: JPMB, MRP, PPN; Analysis and interpretation of the data: JPMB, MRP; Drafting, revision, approval of the submitted manuscript: JPMB, MRP.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Sat 19, Jun 2021Accepted: Thu 19, Aug 2021
Published: Thu 02, Sep 2021
Copyright
© 2023 Jose Pablo Martinez Barbero. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JBN.2021.01.01
Author Info
Jose Pablo Martinez Barbero M. Revelles-Paniza P. Perez-Naranjo
Corresponding Author
Jose Pablo Martinez BarberoNeuroimaging Section, Radiology Service, Hospital Universitario Virgen de las Nieves, Granada, Spain
Figures & Tables
References
1.
Roy
D, Rao PJ, Phan K, Mobbs RJ, Selby M (2016) Spinal cord compression from
Wegener’s granulomatosis: an unusual presentation. J Spine Surg 2:
319-323. [Crossref]
2. Bachmeyer C, Cervera P, Marro B, Ammouri W, Bouvard E et al. (2007) Thoracic spinal cord compression indicating Wegener’s granulomatosis in a patient with a previous presumptive diagnosis of microscopic polyangiitis. Joint Bone Spine 74: 382-384. [Crossref]
3. Nishino H, Rubino FA, DeRemee RA, Swanson JW, Parisi JE (1993) Neurological involvement in Wegener's granulomatosis: an analysis of 324 consecutive patients at the Mayo Clinic. Ann Neurol 33: 4-9. [Crossref]
