Spread of SARS-CoV-2 (COVID-19) in a High-Volume Hospital: Vascular Surgery Impact
A B S T R A C T
Increasing population rates of coronavirus disease 2019 (COVID-19) are occurring in several countries and continents. The impact regarding vascular activity, consequences and complication is scarce and makes the future perspective unclear. The aim of this report is to describe the changes in a high-volume University Hospital, relevant for future decisions. The mortality and morbidity should be higher not only in COVID+ patients but also in vascular patients.
Keywords
Coronavirus disease, vascular patients, vascular activity, population rates, future perspective unclear, volume surgery
Introduction
The widespread and high rate of viral infection have made it necessary to elaborate adequate strategy on the issue, facing surgical departments during the COVID-19 pandemic. The points of interest on which to focus attention were directed to a redistribution of resources and priority classes. The first decision is to divide the healthcare building in COVID and non COVID area/hospital; then, give priority to the diseases to be treated within the framework, favoring only those that are serious and life-threatening or those with a high risk of disability, developing a cohesive leadership team and system for frequent communication throughout the department, ensuring adequate hospital capacity to care for an anticipated influx of COVID-19 patients, safeguarding supplies of blood products and personal protective equipment to protect patients and all staff working in the hospital.
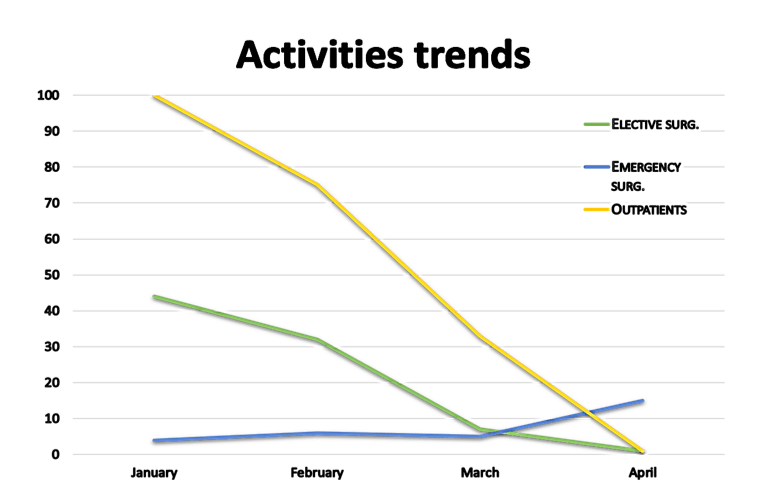
Therefore, it was essential to reduce the elective activities and surgical practice in the various specialities to ensure the necessary resources in the management of the spread of the related COVID-19 pathology; these measures led to a drastic reduction in non-essential activities related to the various branches with a clear polarization in COVID-19 hospitals dedicated to emergency activities as can be observed in the last quarter also in our center. As a consequence, the trend of the pandemic in Italy had a dramatic inversely proportional trend on vascular surgical activity (Table 1).
To cope with an unprecedented emergency since World War II, scientific societies quickly updated behavioural guidelines. Numerous specialists are involved in the elaboration of the guidelines that may be of interest for vascular surgery, which must consider both the aspects of prevention of the spread of the disease and the health of the patient in an emergency condition. They are listed in (Table 2). In our experience, treatment protocols have been implemented which involved the hospital in the division into COVID and non-COVID areas, the implementation of personnel and patient protection protocols, antibiotic prophylaxis and anaesthesiological management of the patient to be operated on carotid CEA surgery. For example, an experience regarding the clinical course of a patient with an indication for an urgent carotid TEA is reported here.
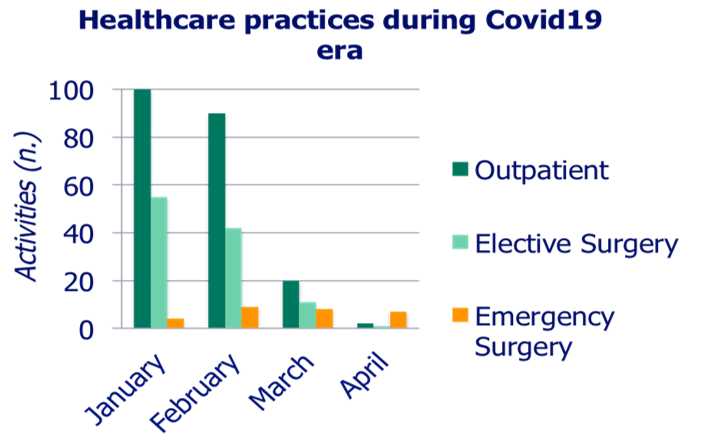
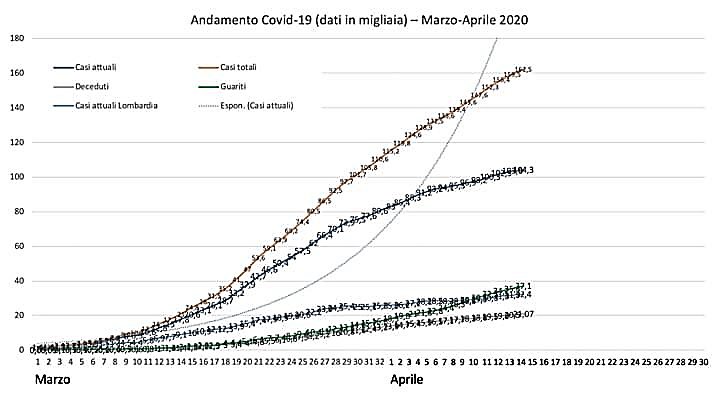
Table 2: Disciplines and methods of involvement.
|
Specialty |
Reason for involvement |
Development of guidelines |
date |
|
Vascular surgery |
Treatment priority |
Management board / SICVE website communication |
22/03/2020 |
|
Infectious diseases |
Adoption of additional precautions for limiting infection and bacterial overlap during hospitalization |
SIMThttps://www.sicp.it/aggiornamento/linee-guida-bp-procedures/2020/05/pandemia-covid-19-cdc/ |
25/06/2020 |
|
Anesthesia |
Pre-intra and postoperative management protocol. |
SIAARTI VAS COVID: vascular approach to the positive COVID-19 patient
http://www.siaarti.it/SiteAssets/News/COVID19%20-%20documenti%20SIAARTI/SIAARTI%20-%20Covid-19%20-%20Controllo%20vie%20aeree%20rev.1.2.pdf |
4/4/2020 |
|
Health management |
The clinical course of the patient from first aid to operating room* |
http://intranetptv/coronavirus/5418-lg-alla-r2.pdf |
23/03/2020 |
* including the hospitalization wards.
Case Report
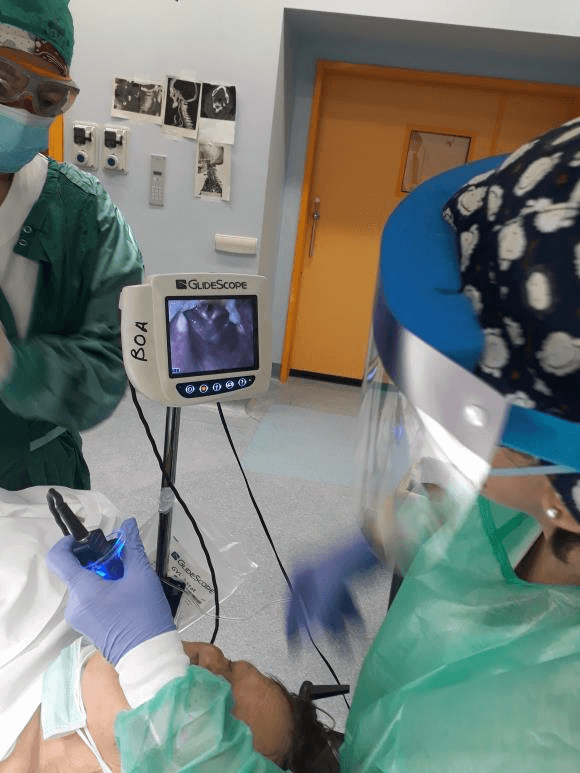
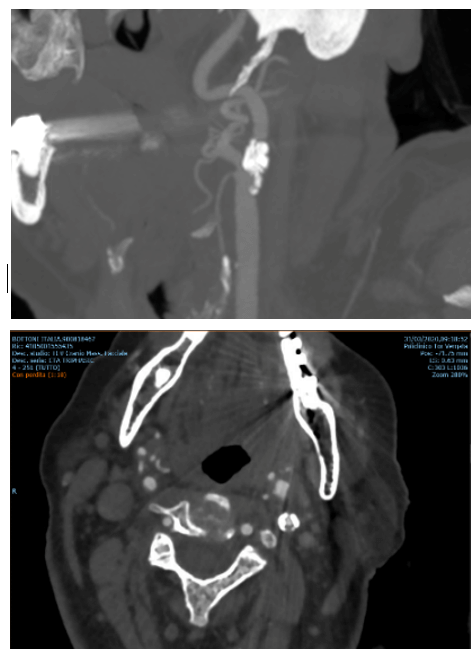
A female 76-year-old, suffering from arterial hypertension in good pharmacological compensation, dyslipidemia, chronic atrial fibrillation in TAO (Sintrom 20 mg). In the anamnesis, no relevant neurological signs or symptoms are associated with transient ischaemic events (TIA). She arrived at the emergency room of our hospital for symptoms compatible with right hemisyndrome with complete facio-brachio-crural plegia, motor aphasia and speech production deficit; she then performed an emergency skull CT that documented the frontal-parietal ischaemic area consistent with the symptomatological framework in progress. Therefore, hospitalization in the NeuroStroke Unit was arranged. The administration of anti-inflammatory and anti-edema therapy with Mannitol 100 mg ev/ die and Corticosteroid brought regression of the symptoms in the following 14 days. For the completion of the diagnostic process, Angio-CT of the neck useful for planning the surgical procedure (Figure 2), brain angio-MRI was performed, which showed absence of Blood-Brain Barrier damage, and Echocolourdoppler of the supra-aortic trunks which documented severe atheromasia of the left carotid axis with mixed component plaque (Grayscale 3) fibrolipid, posteriorly ulcerated and determining stenosis of about 75% of endoluminal vessel diameter according to NASCET criteria. In relation to plaque instability and the possibility of a new emboligenic source congruent to the previously described lesion, following a stabilization from the neurological and general aspects, it was subjected to carotid endarterectomy. The anaesthesiological management has provided for the use of the GlideScope AVL®, with the aim of reducing the proximity of the operator from the introduction of the endotracheal tube. (Figure 1). An endarterectomy with a standard technique was the procedure which was compatible with the new SICVE indications that frame the symptomatic stenoses of the carotid artery in the risk categories according to the European and WHO new guidelines.
Figure 1: Intraoperative cautions. The use of the Glidescope ® system moves the anesthesiologist away from the mouth, limiting proximity to the patient when she opens the mouth. The operating team takes the necessary precautions. There is an eye barrier and two protection layers: (normal surgical masks and FFP2 ) during surgery.
Figure 2: Triphasic CTA with multiplanar reconstruction of LCA, showing calcified lesion with fresh thrombus in a posterior wall of the artery.
Discussion
The treatment of a patient suffering from other urgent pathology in a COVID-19 Hospital requires the application of new prevention and protection hygiene-health procedures through new multidisciplinary measures. In order to avoid contagion by healthcare personnel, the dedicated team needs a preliminary infectious disease screening consisting of a gold-pharyngeal swab and a blood sample. When setting up and preparing materials inside the operating room, pay attention to the number of operators required and the distance between them, when possible; the protection of all staff employed is increased with the use of multilayer devices, an overlap of the inhaled and exhaled air filter devices (FFP 2 and 3 + surgical masks) and use of visors or safety goggles. With the purpose to reduce the exposure to the patient’s Flugge microdroplets and particulates, during the anaesthesiological induction and intubation phase, is evident the need to increase the operator-patient distance by using glides or tracheal cannulas of greater length and interposing a layer disposable of plastic protector that interrupts the contiguity of the exhaled elements.
In line with the new indications for surgical procedures and the recent measures outlining behavioural models to be followed to decrease the risk of contagion, there is a need to develop centers dedicated to the treatment of COVID-19 in the area with consequent limitation of resources for this function (Figure 3). Services such as outpatient activities, first-level diagnostic services and instrumental follow-ups of patients with chronic pathological conditions or previously undergoing surgery are suspended. Elective surgical activity is put on standby; cases in need of timely treatment are redistributed throughout the territory in dedicated non-COVID-19 hospitals. The emergency channel has instead preserved the urgency, after careful evaluation during triage and after stabilization of the framework, where possible, is transferred to another center. Therefore, the drastic reduction of activities in a quantitative and qualitative sense is evident.
Figure 3: Activities trends of the first quarter of 2020.
Conclusion
In the current era dominated by the spread and constant increase of COVID-19-positive cases, the symptomatic variability of the pathology imposes the need to create dedicated alternative healthcare facilities on the territory. The marked limitations of the indications and treatment possibilities of specialist surgeries are based on the rationale of avoiding the saturation of aids and places in intensive care, which are reserved for the treatment of this pathology allowing the turnover of the anaesthesiological staff and simultaneously reducing the biological risk for all personnel involved. Currently only the surgical activity of the treatment of neoplastic pathology is maintained; the second available channel is the one reserved for the emergency. Probably the indispensable activity of specialist surgeries will be decentralized with the possibility of using dedicated facilities at other centers after careful screening and monitoring of the conditions of the operators. If this evolution continues over time, an increase in mortality from cardiovascular-related diseases can be expected.
Consent
All study participants provided informed consent.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 09, Jul 2020Accepted: Thu 23, Jul 2020
Published: Mon 10, Aug 2020
Copyright
© 2023 Andrea Ascoli Marchetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GSCR.2020.02.01
Author Info
Andrea Ascoli Marchetti Ciattaglia Riccardo Dauri Mario Giuliano Ilaria Sarmati Loredana Ippoliti Arnaldo
Corresponding Author
Andrea Ascoli MarchettiVascular Surgery Unit, Biomedicine and Prevention Department, University of Rome Tor Vergata, Rome, Italy
Figures & Tables
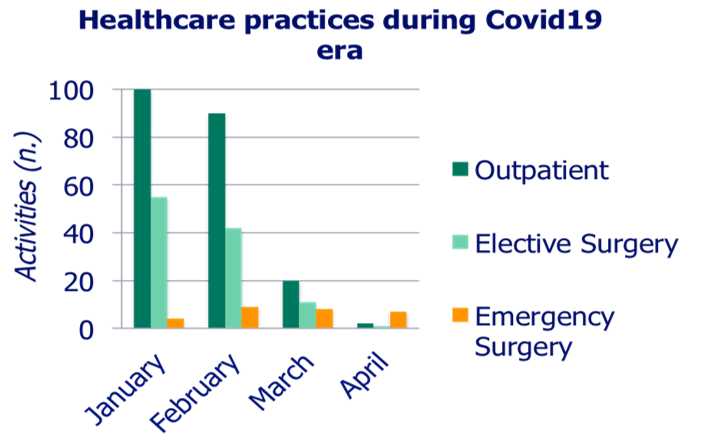
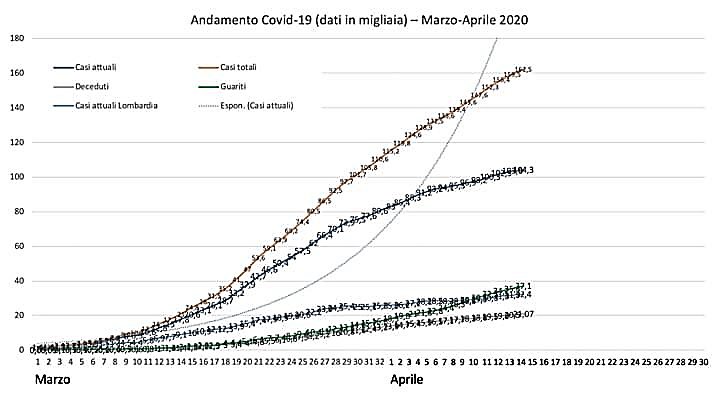
Table 2: Disciplines and methods of involvement.
|
Specialty |
Reason for involvement |
Development of guidelines |
date |
|
Vascular surgery |
Treatment priority |
Management board / SICVE website communication |
22/03/2020 |
|
Infectious diseases |
Adoption of additional precautions for limiting infection and bacterial overlap during hospitalization |
SIMThttps://www.sicp.it/aggiornamento/linee-guida-bp-procedures/2020/05/pandemia-covid-19-cdc/ |
25/06/2020 |
|
Anesthesia |
Pre-intra and postoperative management protocol. |
SIAARTI VAS COVID: vascular approach to the positive COVID-19 patient
http://www.siaarti.it/SiteAssets/News/COVID19%20-%20documenti%20SIAARTI/SIAARTI%20-%20Covid-19%20-%20Controllo%20vie%20aeree%20rev.1.2.pdf |
4/4/2020 |
|
Health management |
The clinical course of the patient from first aid to operating room* |
http://intranetptv/coronavirus/5418-lg-alla-r2.pdf |
23/03/2020 |
* including the hospitalization wards.
References
- Lancaster EM, Sosa JA, Sammann A, Pierce L, Shen W (2020) Rapid Response of an Academic Surgical Department to the COVID-19 Pandemic: Implications for Patients, Surgeons, and the Community. J Am Coll Surg 230: 1064-1073. [Crossref]
- World Health Organization. Coronavirus disease (COVID-19) situation reports.
- Aiello A, Anichini R, Brocco E, Caravaggi C, Chiavetta A (2014) Treatment of peripheral arterial disease in diabetes: a consensus of the Italian Societies of Diabetes (SID, AMD), Radiology (SIRM) and Vascular Endovascular Surgery (SICVE). Nutr Metab Cardiovasc Dis 24: 355-369. [Crossref]
- American College of Surgeons. COVID-19: Recommendations for Management of Elective Surgical Procedures.
- Ng JJ, Ho P, Dharmaraj RB, Wong JCL, Choong AMTL (2020) The Global Impact of COVID-19 on Vascular Surgical Services. J Vasc Surg 71: 2182.e1-2183.e1. [Crossref]
- García-Pastor A, Gil-Núñez A, Ramírez-Moreno JM, González-Nafría N, Tejada J et al. (2020) Progression of carotid near-occlusion to complete occlusion: related factors and clinical implications. J Neurointerv Surg. [Crossref]
- Wenlong Yao, Tingting Wang, Bailing Jiang, Feng Gao, Li Wang et al. (2020) Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth 125: e28-e37. [Crossref]
- Naylor AR, McCabe DJH (2020) New Data and the Covid-19 Pandemic Mandate a Rethink of Antiplatelet Strategies in Patients With TIA or Minor Stroke Associated With Atherosclerotic Carotid Stenosis. Eur J Vasc Endovasc Surg 59: 861-865. [Crossref]
- Viguier A, Delamarre L, Duplantier J, Olivot J, Bonneville F (2020) Acute Ischemic Stroke Complicating Common Carotid Artery Thrombosis During a Severe COVID-19 Infection. J Neuroradiol. [Crossref]
- Hellegering J, van der Laan MJ, Heide EJ, Uyttenboogaart M, Zeebregts CJ et al. (2020) Preventing stroke in symptomatic carotid artery disease during the COVID-19 pandemic. J Vasc Surg 72: 755-756. [Crossref]
- Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I et al. (2020) COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol 75: 2950-2973. [Crossref]
