Standard Surgical Excision of Basal Cell Carcinomas in the Non-H Area of the Face: A Case Series Illustrating an Alternative to Mohs Micrographic Surgery
A B S T R A C T
Introduction: Basal cell carcinoma (BCC) is the most common cutaneous malignancy among Caucasians. Most studies compare the efficacy of standard surgical excision versus Mohs micrographic surgery (MMS) for the treatment of non-melanoma skin cancers in the high-risk or H area of the face. This case series focuses on the lesser-studied non-H area and suggests the use of standard surgical excision as an alternative to MMS for these regions of the face.
Methods: A total of 10 patients with BCCs of the non-H area of the face underwent standard surgical excision with repair at the James A. Lovell Federal Health Center between October 2014 to October 2018. The average age of this group was 77.3 years and all patients were males. Nine of the 10 patients had nodular type BCCs and 1 patient had micronodular type BCC with ulceration. BCCs were located on the forehead in 8 cases and the cheek in 2 cases. Diameters of the lesions ranged from 6mm-8mm. Excision margins were 3- to 5-mm. Defects were repaired using local flaps in 9 cases and linear closure in 1 case.
Results: Histopathologic evaluation of the excision specimens revealed clear surgical margins in 9 out of 10 cases. There was one case in which positive deep margins were identified, although the patient had a BCC with a more aggressive histologic pattern. Of the 9 cases with clear surgical margins, none had clinical evidence of local recurrence at follow-up ranging from 2 to 38 months.
Discussion: BCCs in the non-H area of the face can be successfully treated using standard surgical excision with a high cure rate and low postoperative complications. MMS should be reserved for BCCs at increased risk for recurrence on the basis of factors such as location in the H area on the face and an aggressive histologic growth pattern (e.g. micronodular, morpheaform, infiltrating, metatypical).
Practice points:
• Basal cell carcinomas in the non-H area of the face can be successfully treated using standard surgical excision with a high cure rate and low postoperative complications.
• Mohs micrographic surgery should be reserved for BCCs at increased risk for recurrence on the basis of factors such as location in the H area on the face and an aggressive histologic growth pattern (e.g. micronodular, morpheaform, infiltrating, metatypical).
Keywords
Basal cell carcinoma, non-melanoma skin cancer, surgical excision
Introduction
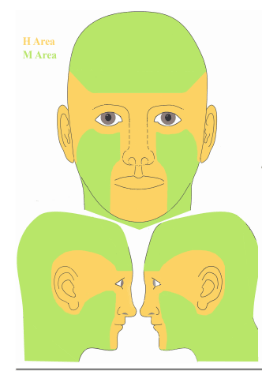
Basal cell carcinoma (BCC) is the most common cutaneous malignancy among Caucasians, and its incidence continues to rise every year [1]. A broad range of therapeutic modalities is available in the treatment of BCCs, including surgical and non-surgical options. Several reports in the literature compare the efficacy of standard surgical excision versus Mohs micrographic surgery (MMS) for the treatment of non-melanoma skin cancers (NMSCs) on the face [2-5]. Most of these studies, however, focus on NMSCs located in the H area of the face which encompasses the “mask areas”- central face, eyelids including inner/outer canthi, eyebrows, nose, lips, chin, ear and periauricular skin/sulci, temple (Figure 1) [6]. MMS is most appropriate for these high-risk regions given their increased propensity for recurrence as compared to the non-H area. Also known as the M area of the face, the non-H area includes the cheeks, forehead, neck, and jawline (Figure 1) [6]. This case series focuses on the lesser-studied non-H area and suggests the use of standard surgical excision as an alternative to MMS for these regions of the face.
Methods
A total of 10 patients with BCCs of the non-H area in the facial region underwent standard surgical excision with repair at the James A. Lovell Federal Health Center between October 2014 to October 2018. All patients with facial BCCs were given the choice of having standard surgery in-house or to be referred to outside physicians for MMS. These 10 patients are consecutive patients. The average age of this group was 77.3 years and all patients were males. Nine of the 10 patients had nodular type BCCs and 1 patient had micronodular type BCC with ulceration. The BCCs were located on the forehead in 8 cases and the cheek in 2 cases. The diameters of the lesions ranged from 6mm to 8mm. Excision margins were the standard 3- to 5-mm margins for BCCs. The resulting defects were repaired using local flaps in 9 cases and with linear closure in 1 case. See (Table 1).
Figure 1: H and M areas of the face [6].
Results
Histopathologic evaluation of the surgical excision specimens revealed clear surgical margins in 9 out of 10 cases. There was 1 case (patient LW) in which positive deep margins were identified, although the patient had a BCC with a more aggressive histologic pattern. In this latter case, the patient declined further surgical intervention, opting for topical treatment with imiquimod and close clinical follow-up. There was no evidence of clinical recurrence noted prior to his death 20 months after the surgical procedure. The remainder of the patients followed up on a regular basis, and none had clinical evidence of local recurrence at follow-up ranging from 2 to 38 months. See (Table 1) and (Figure 2).
Table 1: Summary of cases.
|
Patient |
Location |
BCC histologic type |
Type of repair |
Surgical margins |
Histopathologic margins |
Recurrence-free duration |
|
MU |
Right forehead |
Nodular |
Bilateral advancement flap |
3mm |
Peripheral: 1mm Deep: 2mm |
12 months |
|
DD |
Left forehead |
Nodular |
Bilateral advancement flap |
5mm |
Peripheral: 8mm Deep: 3mm |
24 months
|
|
LW |
Right forehead |
Micronodular with ulceration |
Bilateral advancement flap |
3mm |
Peripheral: 3mm Deep: + |
20 months |
|
RH |
Right forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 4mm Deep: 3mm |
10 months |
|
MJ |
Left cheek |
Nodular |
Single rotational flap |
4mm |
Peripheral: 4mm Deep: 3mm |
4 months |
|
TB |
Right forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 3mm Deep: 2.5mm |
38 months
|
|
RD
|
Left forehead |
Nodular |
O-to-Z flap |
4mm |
Peripheral: 2mm Deep: 2mm |
5 months |
|
LP
|
Mid-forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 3mm Deep: 1mm |
5 months |
|
GP
|
Left forehead
|
Nodular |
Unilateral advancement flap |
4mm |
Peripheral: 2.5mm Deep: 1.5mm |
5 months |
|
JS
|
Left cheek
|
Nodular |
Linear closure |
4mm |
Peripheral: 3mm Deep: 3mm |
2 months |
Figure 2: Representative case: nodular BCC on the left forehead excised and repaired with a bilateral advancement flap (Patient DD).
(A) Preoperative marked clinical photograph. (B) Immediate post-operative clinical photograph. (C) Postoperative clinical photograph at 17-month follow-up. (D) Postoperative clinical photograph at 24-month follow-up.
Discussion
The main goal in the management of NMSCs is to treat the cancer with adequate surgical margins while preserving maximal function and cosmesis. This is of particular importance for the facial region. The two most widely utilized therapeutic options for facial NMSCs are standard surgical excision and MMS. It is generally accepted that standard surgical excision with adequate surgical margins provides up to 95% cure rate with low-risk NMSCs, whereas high-risk BCCs located in the H area of the face as well as BCCs with an aggressive histologic type meet the indication for MMS [7]. A 2012 retrospective study evaluated the efficacy of standard surgical excision versus MMS in the non-H-zone of the face [8]. This study reviewed a total of 588 cases, of which 289 patients had non-H-zone, extremity, and trunk lesions. Overall recurrence rates of standard surgical excision and MMS at 3-year follow-up were not statistically different between the two groups (4.8% and 3% respectively). The results of their study suggested that patients with NMSCs in non-premium areas of the body may be more effectively treated with standard surgical excision rather than MMS. Other than this study, there is a relative paucity of data in the literature with regard to the clinical efficacy of standard surgical excision versus MMS in the non-H area of the face.
The intent of this case series is not to compare the efficacy of both treatment modalities, but our purpose is to support the role for standard surgical excision as an alternative to MMS in the treatment of non-histologically aggressive BCCs in the non-H area of the face. All patients in our study had BCCs that were not located in high-risk anatomic areas. Only one patient had a BCC with a more aggressive histologic growth pattern, and deep surgical margins were positive in this case. There was no evidence of clinical recurrence in any of the patients during the follow-up time period, which ranged from 2 to 38 months post-procedure. This does identify a limitation of the current study, which is the length of the follow-up time period. It would be ideal to follow these patients for a longer duration of time given that BCCs have slow rates of growth and recurrences are frequently diagnosed beyond 5 years following definitive treatment9. However, histological clearance as demonstrated by formalin-fixed paraffinized sections should provide a very good indication of complete surgical removal of BCCs.
Additional factors that favor standard surgical excision over MMS include the fact that MMS is both time-consuming and labor-intensive, and the surgical technique can incur a higher cost. Another important factor to consider, particularly for our veteran patient population, is the issue of access to on-site MMS services. A 2009 study utilizing an email survey sent to 101 Veterans Health Administration Hospitals in the United States with Dermatology Services found that veteran access to MMS is not uniform across the country. In fact, on-site MMS is only available at 11 Veterans Affairs (VA) hospitals spanning nine states [10]. Thus, many veterans are unable to benefit from the convenience of on-site MMS, and they are sent to an off-site location for MMS at the majority of VA hospitals [10]. Standard surgical excision, in contrast, can be performed on-site and is less expensive as well as less time- and resource-intensive than MMS.
Based on our experiences with excision of non-H area BCCs on the face, we conclude that BCCs in these facial regions can be successfully treated using standard surgical excision with high cure rate and low postoperative complications. MMS should be reserved for BCCs at increased risk for recurrence on the basis of factors such as location in the H area on the face and an aggressive histologic growth pattern (e.g. micronodular, morpheaform, infiltrating, metatypical). Additional studies with larger sample sizes and a head-to-head comparative study design are necessary to accurately assess the treatment superiority of standard excision compared to MMS in these lesser-studied areas on the face.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 02, Oct 2019Accepted: Tue 15, Oct 2019
Published: Thu 31, Oct 2019
Copyright
© 2023 Stephanie Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2019.05.10
Author Info
J Au LS Chan O Lai Stephanie Wang
Corresponding Author
Stephanie WangDepartment of Dermatology (MC 624), University of Illinois at Chicago, 808 S Wood St, Room 380 CME, Chicago
Figures & Tables
Table 1: Summary of cases.
|
Patient |
Location |
BCC histologic type |
Type of repair |
Surgical margins |
Histopathologic margins |
Recurrence-free duration |
|
MU |
Right forehead |
Nodular |
Bilateral advancement flap |
3mm |
Peripheral: 1mm Deep: 2mm |
12 months |
|
DD |
Left forehead |
Nodular |
Bilateral advancement flap |
5mm |
Peripheral: 8mm Deep: 3mm |
24 months
|
|
LW |
Right forehead |
Micronodular with ulceration |
Bilateral advancement flap |
3mm |
Peripheral: 3mm Deep: + |
20 months |
|
RH |
Right forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 4mm Deep: 3mm |
10 months |
|
MJ |
Left cheek |
Nodular |
Single rotational flap |
4mm |
Peripheral: 4mm Deep: 3mm |
4 months |
|
TB |
Right forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 3mm Deep: 2.5mm |
38 months
|
|
RD
|
Left forehead |
Nodular |
O-to-Z flap |
4mm |
Peripheral: 2mm Deep: 2mm |
5 months |
|
LP
|
Mid-forehead |
Nodular |
Bilateral advancement flap |
4mm |
Peripheral: 3mm Deep: 1mm |
5 months |
|
GP
|
Left forehead
|
Nodular |
Unilateral advancement flap |
4mm |
Peripheral: 2.5mm Deep: 1.5mm |
5 months |
|
JS
|
Left cheek
|
Nodular |
Linear closure |
4mm |
Peripheral: 3mm Deep: 3mm |
2 months |
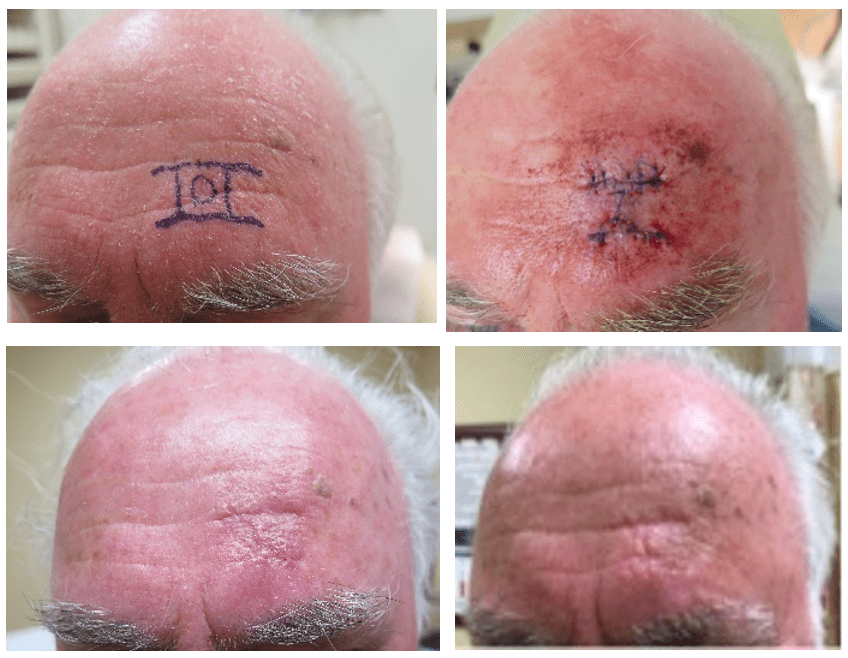
(A) Preoperative marked clinical photograph. (B) Immediate post-operative clinical photograph. (C) Postoperative clinical photograph at 17-month follow-up. (D) Postoperative clinical photograph at 24-month follow-up.
References
- Smeets NW, Kuijpers DI, Nelemans P, Ostertag JU, Verhaegh ME et al. (2004) Mohs’ micrographic surgery for treatment of basal cell carcinoma of the face – results of a retrospective study and review of the literature. Br J Dermatol 151: 141-147. [Crossref]
- Mosterd K, Krekels GA, Nieman FH, Ostertag JU, Essers BA et al. (2008) Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol 9: 1149-1156. [Crossref]
- van Loo E, Mostern K, Krekels GA, Roozeboom MH, Ostertag JU et al. (2014) Surgical excision versus Mohs’ micrographic surgery for basal cell carcinoma of the face: A randomised clinical trial with 10 year follow-up. Eur J Cancer 50: 3011-3020. [Crossref]
- Smeets NW, Krekels GA, Ostertag JU, Essers BA, Dirksen CD et al. (2004) Surgical excision vs. Mohs’ micrographic surgery for basal cell carcinoma of the face: randomised controlled trial. Lancet 364: 1766-1772. [Crossref]
- Muller FM, Dawe RS, Moseley H, Fleming CJ et al. (2009) Randomized comparison of Mohs micrographic surgery and surgical excision for small nodular basal cell carcinoma: tissue-sparing outcome. Dermatol Surg 35: 1349-1354. [Crossref]
- Blechman AB, Patterson JW, Russell MA (2014) Application of mohs micrographic surgery appropriate-use criteria to skin cancers at a university health system. J Am Acad Dermatol 71: 29-35. [Crossref]
- Ad Hoc Task Force, Connolly SM, Baker DR, Coldiron BM, Fazio MJ et al. (2012) AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol 67: 531-550. [Crossref]
- Pereira CT, Kruger EA, Sayer G, Kim J, Hu J et al. (2013) Mohs versus surgical excision in nonmelanoma skin cancers: does location matter? Ann Plast Surg 70: 432-433. [Crossref]
- Kim JYS, Kozlow JH, Mittal B, Moyer J, Olencki T et al. (2018) Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol 78: 540-559. [Crossref]
- Karen JK, Hale EK, Nehal KS, Levine VJ (2009) Use of Mohs surgery by the Veterans Affairs Health Care System. J Am Acad Dermatol 60: 1069-1070. [Crossref]
