Streptococcus intermedius Splenic Abscess in a Child: Case Report and Review of the Literature
A B S T R A C T
Objective: We report a case of Streptococcus intermedius splenic abscess and review of relevant literature.
Design: A retrospective report and review of the English literature concerning splenic abscess cause by Streptococcus intermedius via PubMed was conducted.
Results: An 8-year-old boy, who presented with fever, abdominal pain, and vomiting, was found to have a large splenic fluid collection. He underwent ultrasound-guided aspiration of the abscess, and the culture grew Streptococcus intermedius. His symptoms and radiographic findings resolved after completion of antibiotics. Isolated splenic abscesses are rare, and this represents the second case in the literature of splenic abscess caused by Streptococcus intermedius.
Conclusion: Streptococcus intermedius is a rare cause of splenic abscess. Isolated splenic abscess requires drainage for both diagnostic and therapeutic purposes.
Keywords
Streptococcus, Spleen, abscess
Introduction
Streptococcus intermedius, along with Streptococcus constellatus and Streptococcus anginosus, are viridans Streptococci belonging to the Anginosus group, formerly classified as the Streptococcus milleri group. These grams positive, catalase negative microaerophilic cocci are reported to be pyogenic organisms and have been implicated in a variety of infections and abscesses, including the brain, meninges, heart, sinuses, liver, lungs, spleen, peritoneum, pelvis, and appendix [1]. S. intermedius has been identified as highly pathogenic and most likely to result in complicated abscess formation. S. intermedius is a normal inhabitant of the oral cavity, respiratory tract and gastrointestinal tract, and abscesses caused by S. intermedius tend to result from hematogenous spread and are traditionally associated with the head, neck and upper chest, and isolated report of spleen involvement [2].
Isolated splenic abscesses are uncommon especially in the pediatric population. Here we describe an otherwise healthy child with multiple, complex splenic abscesses caused by S. intermedius, an unusual pathogen only implicated once prior in an isolated splenic abscess in an infant. We subsequently review and discuss the available literature for management of this infection.
Case Description
An 8-year-old male presented to the emergency department with a two-week history of persistent fever, left sided abdominal pain, difficulty breathing and chest pain. One week prior, he had been seen three times in the emergency department and once by his general pediatrician for similar complaints. Previous work up was significant for heterogeneous splenic lesions on computed tomography (CT) scan presumed to be splenic lacerations in the setting of left sided abdominal trauma from a soccer ball. He was briefly admitted for serial abdominal exams and laboratory monitoring, and discharged home after two days.
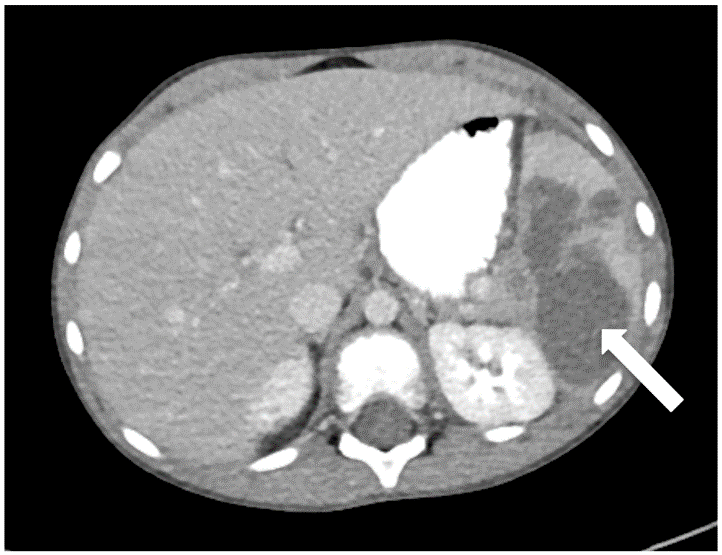
At current presentation, he was toxic appearing and writhing in pain. He was afebrile but tachycardic, with labs significant for leukocytosis with white blood cell (WBC) of 14.4x10e3cells/µL with 87% neutrophils, hemoglobin of 9.0 g/dL and elevated sedimentation rate (ESR) and C-reactive protein (CRP) of 96 mm/h and 8.9 mg/dL, respectively. Repeat abdominal CT scan demonstrated similar findings to his prior exam with a new presence of focal fat stranding around the splenic flexure (Figure 1A). He was given a one-time dose of intravenous (IV) ampicillin/sulbactam for possible diverticulitis, and empiric therapy was initiated with IV ceftriaxone and metronidazole following hospitalization.
The patient had no recent illness, dental work, recent travel, dietary or animal exposures and was up to date with his vaccinations. He had no history of recurrent or frequent infections. Given the presence of leukocytosis, elevated inflammatory markers, and the development of persistent fever, the working diagnosis was an infected splenic hematoma or abscess. On hospital day one, he underwent ultrasound-guided aspiration of his splenic fluid collections with subsequent drain placement. The resulting purulent fluid was sent for analysis with gram stain, aerobic, anaerobic and fungal cultures. The fluid culture yielded gram-positive rods that were later identified as S. intermedius, and all other surgical cultures were negative. The remainder of his infectious work up including serologies for Epstein-Barr virus, cytomegalovirus, Echinococcus, Bartonella and Brucella titers, blood-based tuberculosis testing with interferon-gamma release assay, and blood and urine cultures all resulted negative.
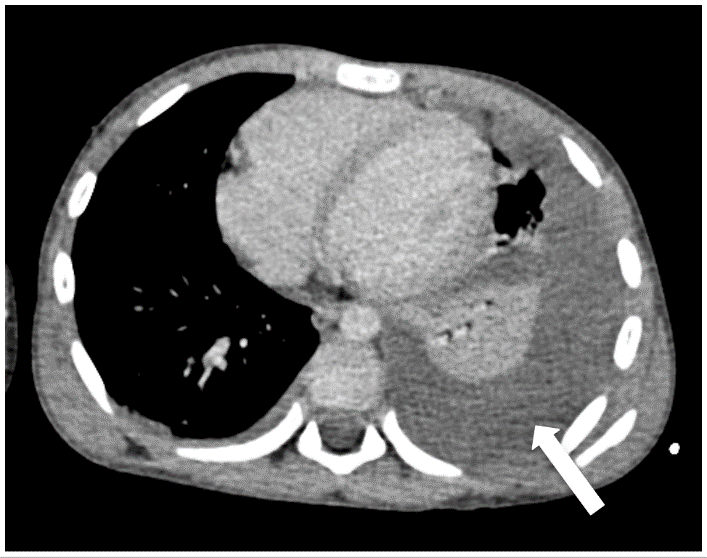
Figure 1: A) Abdominal CT imaging demonstrating subscapular hypodensities measuring 7.2 x 3.9 cm in the lower pole of the spleen (arrow). B) Chest CT scan showing moderately large pleural effusion (arrow).
An immune evaluation including immunoglobulins, antibody response to diphtheria/tetanus/Haemophilus influenzae/Streptococcus pneumoniae, lymphocyte enumeration including T, B, and NK cells, and neutrophil oxidative burst were normal. His early hospital course was complicated by intermittent episodes of desaturations requiring supplemental oxygenation, ultimately leading to the discovery of left-sided pleural effusion (Figure 1B). Otherwise, the remainder of his hospital course was unremarkable. The S. intermedius isolate susceptibilities demonstrated sensitivity to levofloxacin, penicillin and vancomycin and resistance to ciprofloxacin. Antimicrobial therapy was deescalated to monotherapy with ceftriaxone.
Prior to discharge, a repeat CT scan was performed to reevaluate his splenic lesions which showed a reduction by approximately 50% of the splenic abscess. Management options were discussed with pediatric surgery, and they identified no indication for splenectomy or surgical intervention for his pleural effusion given his clinical improvement. A peripherally inserted central catheter was placed for long-term IV antibiotic therapy and he was discharged home on hospital day eleven. Overall, the patient completed 28 days of IV ceftriaxone followed by two weeks of oral amoxicillin. The WBC, ESR, and CRP had normalized. Follow up CT scan of the chest and abdomen showed resolution of the splenic abscess and pleural effusion.
Discussion
Splenic abscesses are particularly uncommon in the pediatric population and may have vague presenting symptoms, such as fever, abdominal pain, left upper quadrant tenderness, leukocytosis and less commonly anorexia, vomiting, left shoulder pain, splenomegaly and pleural effusion [3]. Thus, a high index of suspicion is required to suspect and diagnose splenic abscesses. Most reported cases of splenic abscesses have been recognized in the setting of metastatic infection such as bacterial endocarditis, immunocompromised states, hemoglobinopathies, secondary infection from splenic trauma or direct extension from infection of contiguous organs [4].
Furthermore, other pathogens known to cause abscesses in the pediatric population include aerobic and facultative bacteria M. tuberculosis, non-typhoidal Salmonella, Bartonella, Brucella, E. coli, S. aureus, and Streptococcus group D, K. pneumonia, Proteus mirabilis and predominant anaerobic bacteria Peptostreptococcus spp., Bacteroides spp., Clostridium spp., Prevotella spp. and Propionibacterium acnes [4]. While our patient had a history of left-sided abdominal trauma from a soccer ball, it is uncertain whether this was the inciting event for his splenic abscess development. However, development of splenic abscesses can be seen as a complication of splenic trauma [5]. Furthermore, due to multiple negative blood cultures and clinical improvement, there was a low suspicion for other sources of infection.
In order to facilitate diagnosis and prevent delays in treatment, abdominal ultrasound (US) and CT scan should be utilized when there is a clinical suspicion for splenic abscess, with CT being the gold standard. Conservative management of splenic abscesses with CT or US guided aspiration/drainage and an appropriate antibiotic coverage has replaced splenectomy in order to preserve splenic function [1, 5]. Percutaneous drainage can be both diagnostic and therapeutic.
While blood cultures can help to isolate pathogens responsible for infection, Faruque et al. noted that only about 50% of blood cultures identified an organism in their analysis of isolated splenic abscesses in children [6]. Thus, a negative blood culture does not exclude the diagnosis or prior transient bacteremia. The patient described in this case exemplifies the importance of microbiological investigation. Without percutaneous drainage and fluid analysis, the responsible pathogen would have gone unrecognized, potentially leaving this patient subject to prolonged course of broad-spectrum antibiotics without a confirmed source of infection.
While S. intermedius is highly pathogenic, the literature supports broad susceptibilities to penicillin, amoxicillin, cefotaxime or ceftriaxone, levofloxacin and vancomycin [7]. While the literature does not have a consensus for the treatment duration of splenic abscesses, the majority of the studies documented treatment for at least two weeks post drainage in the setting of improved clinical picture.
Conclusion
Isolated splenic abscesses are uncommon in the pediatric population and require a high index of suspicion for diagnosis. On the basis of review of the literature and our experience, diagnosis should be performed with abdominal CT scan, completed early in the clinical presentation to facilitate diagnosis and treatment. We recommend utilizing conservative management with CT or US guided aspiration/drainage to preserve splenic function and an appropriate antibiotic coverage based on microbiological susceptibilities. Here we describe a case in which we followed the aforementioned clinical management and the patient’s clinical outcome was favorable.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Sat 14, Mar 2020Accepted: Mon 06, Apr 2020
Published: Tue 14, Apr 2020
Copyright
© 2023 Niraj Patel. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.02.01
Author Info
Corresponding Author
Niraj PatelDepartment of Pediatrics, Section of Infectious Disease and Immunology, Levine Children’s Hospital, Atrium Health, Charlotte, North Carolina, USA
Figures & Tables
References
- Livingston LV, Perez Colon E (2014) Streptococcus intermedius Bacteremia and Liver Abscess following a Routine Dental Cleaning. Case Rep Infect Dis 2014: 954046. [Crossref]
- Matsubayashi T, Matsubayashi, Saito I, Tobayama S, Machida H (2007) Splenic abscess in an infant caused by Streptococcus intermedius. J Infect Chemother 13: 423-425. [Crossref]
- Maliyil J, Caire W, Nair R, Bridges D (2011) Splenic abscess and multiple brain abscesses caused by Streptococcus intermedius in a young healthy man. Proc (Bayl Univ Med Cent) 24: 195-199. [Crossref]
- Brook I, Frazier EH (1998) Microbiology of liver and spleen abscesses. J Med Microbiol 47: 1075-1080. [Crossref]
- Frumiento C, Sartorelli K, Vane D (2000) Complications of splenic injuries: expansion of the nonoperative theorem. J Pediatr Surg 35: 788-791. [Crossref]
- Furuichi M, Horikoshi Y (2018) Sites of infection associated with Streptococcus anginosus group among children. J Infect Chemother 24: 99-102. [Crossref]
- Faruque AV, Qazi SH, Arshad M, Anwar N (2013) Isolated splenic abscess in children, role of splenic preservation. Pediatr Surg Int 29: 787-790. [Crossref]
