Successful Treatment of Dual Juxtahepatic Inferior Vena Cava Injuries Using Formal Atriocaval Shunt: A Case Report and Review of the Literature
A B S T R A C T
Repair of penetrating retrohepatic inferior vena cava (IVC) injuries continues to challenge trauma surgeons due to difficulty in accessing the injury, hemorrhage prior to the repair, and associated high mortality rates. Complication by suprahepatic vena cava injuries portends an increased risk of an unfavorable outcome. Over time, overall survival has been relatively unchanged, and the morbidity and mortality associated with these injuries continue to be very high. First proposed by Shrock et al. in 1968, atriocaval shunt placement remains the gold standard approach for the temporary bypass of these lesions by controlling bleeding from the retrohepatic IVC to allow time for repair prior to exsanguination and death. Despite familiarity with this management strategy for decades, these injuries remain infrequent but continue to have poor survival due to their complexity. There are only rare examples of the use of this approach resulting in successful discharge from the hospital. We present a case report of survival after the successful deployment of an atriocaval shunt in a patient who sustained multiple gunshot wounds to his right thoraco-abdomen, left chest, and upper and lower extremities. He ultimately survived to discharge from the hospital. We provide a brief review of the current literature and propose future approaches to repairs of juxtahepatic IVC injuries.
Keywords
Atriocaval shunt, retrohepatic inferior vena cava injury, schock shunt, hemorrhagic shock
Introduction
Retrohepatic and suprahepatic IVC and hepatic venous injuries are rare but lethal lesions. They are notoriously difficult to repair due to their complicated anatomic location resulting in exsanguination prior to being able to obtain vascular control. The first large study examining these injuries revealed an associated mortality rate of up to 81% [1]. Due to the excess mortality related to these injuries, various approaches have been developed and proposed for their repair. In managing complex hepatic injuries with rapid exsanguination, the first step is generally control of the vascular inflow via temporary occlusion of the hepatoduodenal ligament resulting in temporary occlusion of the portal vein and hepatic artery (more commonly known as the Pringle maneuver). However, subsequent steps vary based on the location of the retrohepatic IVC injury and operating surgeon experience. Arguably, the most commonly accepted technique for vascular shunting of the retrohepatic IVC is the atriocaval shunt (ACS), which was first described by Schrock et al. in 1968 [2]. Though technically challenging, the technique requires limited resources and thus allows for expeditious placement of the shunt without using the endovascular intervention. Vascular isolation is often challenging in the setting of acute severe polytrauma, where simultaneous addressing of multiple injuries is required to prevent mortality in the patient.
We report the successful placement and use of an ACS after multiple gunshot wounds resulting in a combined retrohepatic and suprahepatic vena caval injury, massive right hemothorax and multiple extremity fractures. Subsequently, we provide a brief overview of the current literature on the treatment of these complex injuries as well as up-and-coming techniques for the repair of these injuries.
Case Report
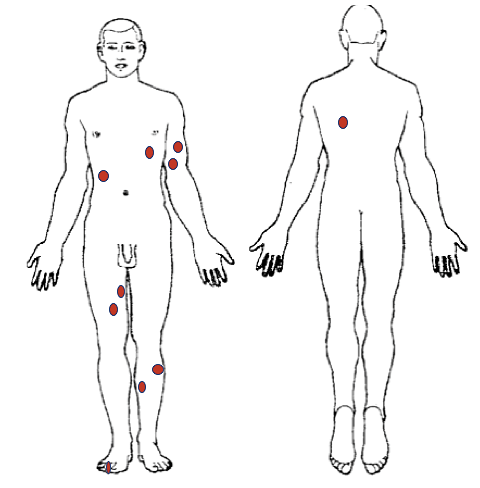
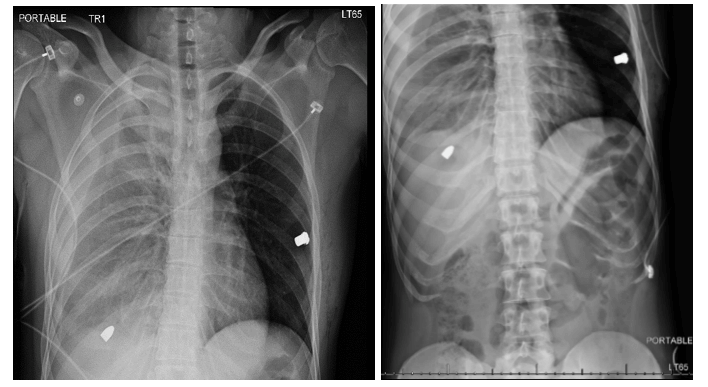
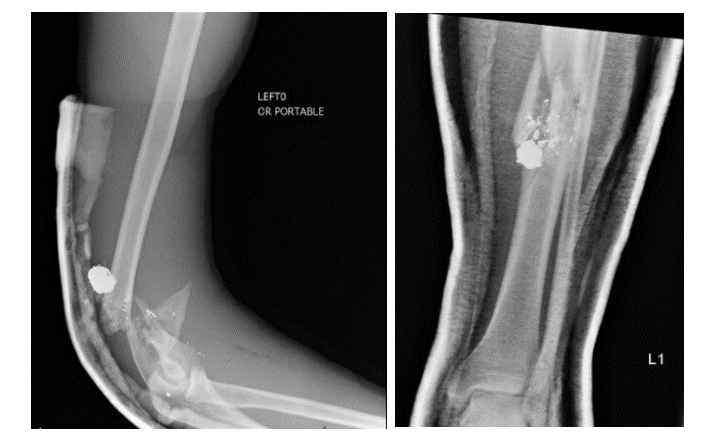
The patient is a 28-year-old man who presented to the trauma center via ground ambulance after sustaining multiple gunshot wounds to the right thoraco-abdomen, left chest, left upper extremity and bilateral lower extremities during a carjacking incident. Upon arrival, he was hypotensive with an initial blood pressure of 90s/60s, and his airway was intact with diminished breath sounds on the right. Although he had palpable femoral pulses bilaterally, he had diminished left pedal pulses. The focused Assessment Sonography for Trauma (FAST) exam was negative for pericardial fluid. The secondary survey revealed gunshot wounds to the left chest just below the nipple, right posterior back, left distal upper arm, right thigh, and through the anterior left lower leg (Figure 1). Initial X-rays revealed a large right hemothorax with a projectile in the right upper quadrant overshadowing the liver as well as ballistic debris within the left chest with no evidence of pneumothorax (Figure 2). In total, the patient sustained eight gunshot wounds with multiple external missile wounds, and four retained metallic foreign bodies. Other injuries depicted below include a comminuted left mid-shaft tibia fracture and a fractured left distal humerus with retained ballistics (Figure 3). His ankle-brachial arterial pressure index (ABI) was diminished to 0.6 on the left and was normal (1.0) on the right.
Figures 1: Diagram of ballistic injuries. Multiple ballistic injuries to the thoracoabdominal cavity, left arm, and bilateral lower extremities.
Figures 2: Chest and abdominal X-rays revealing left pneumothorax and multiple ballistic fragments in the thorax and abdominal cavities.
Figures 3: Left inset: Left upper extremity X-ray revealing retained ballistic and left distal humeral fracture. Right inset: Left lower extremity X-ray revealing complex ballistic left tibial mid-shaft fracture with retained ballistic fragment.
Given the concern for major thoraco-abdominal injuries in the setting of hypotension and a suspected right diaphragm injury with a massive right hemothorax, the trauma team activated the massive transfusion protocol (MTP) and took the patient to the operating room expeditiously. Placement of a right chest tube yielded immediate evacuation of one liter of blood. Based on the suspected trajectory of the missile and radiographic finds, exploratory laparotomy provided the best initial operative approach. Mobilization of the right lobe of the liver revealed massive hemorrhage from behind the dome of the liver at the level of the diaphragmatic hiatus. A Pringle maneuver reduced some of the retrohepatic bleeding.
While packing the liver with laparotomy pads, an extension of the midline abdominal incision to above the sternal notch using a median sternotomy approach exposed the dome of the liver and retrohepatic portion of the IVC. We then performed an atriotomy after placing a purse-string in the right atrial appendage followed by atriocaval shunt placement using a formal Schrock shunt with a silastic balloon. Passage of the device below the level of the retrohepatic vena cava injury but above the renal veins with inflation of the balloons successfully isolated the hemorrhage. Compression of the supraceliac aorta helped to decrease the perihepatic bleeding, maintain coronary and cerebral perfusion, and improve the patient’s hemodynamics. The division of the right diaphragm provided direct access to the IVC injury.
The detachment of the hepatic ligaments and further mobilization of the right lobe of the liver allowed for the identification of the large ballistic defect in the anterolateral suprahepatic IVC. Slow, gradual withdrawal of the shunt allowed for the placement of a side-biting vascular clamp over the vascular defect. Closure of the 7 mm defect primarily using 5-0 Prolene suture provided preliminary hemostasis with the assistance of vascular surgery. However, after further retraction of the Schrock shunt, we identified a second 6 mm posterior retrohepatic IVC injury and controlled it in a similar fashion. Exploration of the right hemithorax through an extension of the diaphragmatic opening revealed a laceration with bleeding from the lower lobe of the right lung. Over-sewing of the lung laceration using a running 5-0 Prolene suture achieved hemostasis.
Upon subsequent abdominal exploration, identification of bleeding from a right lower lobe liver laceration required over-sewing to stop the hemorrhage. After achieving adequate hemostasis of the liver, we repaired the right diaphragmatic defect using 2-0 PDS suture as well as closed the median sternotomy over drains using K-wires. Bilateral chest tubes, mediastinal and perihepatic drain placement facilitated monitoring for evidence of clinically significant bleeding postoperatively. Of note, after the achievement of hemostasis, an on-table angiography revealed vasospasm of the left lower extremity arterial system but no frank vascular injury. The patient’s fractures of the left upper and lower extremities required splint placement (Figure 3). After resuscitation in the ICU, the patient was successfully extubated on post-operative day one after open reduction and internal fixation of his left tibia fracture. The ICU team transferred him to the floor on POD-5 in stable condition. His hospital course was relatively uncomplicated, except for the development of a small pulmonary embolism, requiring treatment with a heparin drip followed by a transition to rivaroxaban (Xarelto) prior to discharge to home on POD-20 in good condition.
Discussion
Retrohepatic inferior vena cava injuries continue to carry a significant risk of mortality due to their difficult-to-access location. The atriocaval shunt (“Shrock Shunt”), a method to control substantial hemorrhage due to hepatic vein, retrohepatic and/or suprahepatic vena cava injuries, remains the gold standard for isolating these injuries in order to provide an opportunity for vascular repair. Initial management of posterior hepatic injuries with suspected retrohepatic IVC injury involves first stopping inflow into the liver via multimodal methods, including compression of the hepatoduodenal ligament, thus diminishing flow into the liver via the portal vein and hepatic artery. When this maneuver fails, injury to the hepatic veins and/or retrohepatic IVC warrants strong consideration and exploration. Proper placement of a large venous shunt to reestablish blood flow across the IVC lesion to the heart to control the retrohepatic sources of bleeding - including the hepatic veins, IVC, right adrenal vein, and inferior phrenic veins - should theoretically stop all bleeding based on anatomical models. Nevertheless, in practice, this maneuver alone may incompletely eliminate the bleeding. Some studies estimate the reduction to be around 40-60% [3].
However, expeditious, correctly executed atriocaval shunt placement used in conjunction with other hemostatic techniques can provide enough reduction of blood flow to allow for repair of the IVC injury prior to exsanguination, as was the case in our patient. Knowledge of this approach as part of the armamentarium of the operative capabilities of the modern trauma surgeon is critical for the surgical provider faced with managing these morbid injuries. Technical difficulty with correctly performing this procedure has been previously described, mainly related to delays in placement due to the requirement for sternotomy and atriotomy, as well as improper placement of the tube without proper occlusion of the retrohepatic vena cava above and below the level of the injury [1]. As such, various alternate techniques proposed for the management of these complex injuries warrant consideration. The first alternative to the ACS is total hepatic vascular isolation (THVI), which involves suprahepatic and infrahepatic IVC occlusion combined with clamping of the hepatoduodenal ligament. Khaneja et al. examined the use of THVI in ten consecutive patients resulting in a reported 70% salvage rate.
In this study, the authors speculate that the worse historical outcomes seen with the atriocaval shunt were due to delays in placement and poor technique. Thus, inadequate experience with the ACS technique may be the primary limitation of its use. The success of the THVI technique is unfortunately highly dependent on the location of the injury and the skill of the trauma surgeon due to difficulty in accessing, occluding and repairing the suprahepatic IVC in a small space. Venovenous bypass, as described in several case reports, is another option to consider [4-6]. This technique uses an extracorporeal circuit to bypass the area of injury with or without the use of an active pump. While allowing completion of the operation in a relatively bloodless field, the requirement for supplementary equipment and additional technical expertise by the on-call surgeon or immediate availability of a cardiothoracic surgeon hampers the use of this procedure.
Recently, an animal study using resuscitative balloon occlusion of the IVC (REBOIVC) showed some promise and improved survival via control of the hepatoduodenal ligament plus the IVC compared to the control of the hepatoduodenal ligament alone [7]. This approach uses a previously developed, commercially available resuscitative, vascular occlusive balloon device to obstruct the IVC internally and regulate bleeding from the injury. Approval by the Food and Drug Administration (FDA) may be forthcoming. This technique is somewhat hindered by requiring this special balloon occlusion device, as well as training in its use, though the device is becoming more commonly available at major trauma centers for its use in occlusion of the aorta. Further studies of this technique are ongoing.
A single case report using IVC stenting for control of a retrohepatic caval injury has been reported as well [8]. With the ready availability of on-table angiography, this may become a viable option depending on the location of the bleeding and access to this limited resource. Despite a variety of strategies for controlling retrohepatic and juxtahepatic venous injuries, surgeon experience with the various techniques and availability of resources appear to be primary drivers of patient outcome. Familiarity with the different techniques and early deployment of the appropriate intervention is essential to improve the patients’ chance of survival.
Conclusion
Due to the unpredictable availability of resources, differences in surgical experience, and limitations associated with each technique used for vascular isolation based on the specific injury, it is important to maintain familiarity with the various management strategies for juxtahepatic IVC injuries in order to maximize patient outcomes. Despite the development of more technologically advanced interventions, the atriocaval shunt maintains its importance in the management of these complex injuries. Familiarity with this technique and early deployment of the atriocaval shunt is essential to improve the chances of survival in this fragile patient population.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Tue 14, Apr 2020Accepted: Mon 04, May 2020
Published: Wed 13, May 2020
Copyright
© 2023 Omar K. Danner. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.05.05
Author Info
Amanda Fobare Brandon Henry Caroline Butler Deepika Koganti Ed Childs Jonathan Nguyen Kahdi Udobi Omar K. Danner Ravi Rajani Richard Sola Ronald Hoard Rondi Gelbard
Corresponding Author
Omar K. DannerMorehouse School of Medicine, Department of Surgery, Atlanta, Georgia, USA
Figures & Tables
References
- Burch JM, Feliciano DV, Mattox KL (1988) The atriocaval shunt: Facts and fiction. Ann Surg 207: 555-568. [Crossref]
- Schrock T, Blaisdell FW, Mathewson C Jr (1968) Management of blunt trauma to the liver and hepatic veins. Arch Surg 96: 698-704. [Crossref]
- Feliciano (2006) Injuries to the great vessels of the abdomen. ACS Surg.
- Horwitz JR, Black T, Lally KP, Andrassy RJ (1995) Venovenous bypass as an adjunct for the management of a retrohepatic venous injury in a child. J Trauma 39: 584-585. [Crossref]
- Thomford NR, Papouras WC, Durzinsky DS (1998) Active venovenous bypass of the retrohepatic vena cava utilizing two atrial cannulae. Am Surg 64: 791-794. [Crossref]
- Baumgartner F, Scudamore C, Nair C, Karusseit O, Hemming A (1995) Venovenous bypass for major hepatic and caval trauma. J Trauma 39: 671-673. [Crossref]
- Reynolds CL, Celio AC, Bridges LC, Mosquera C, OʼConnell B et al. (2017) REBOA for the IVC? Resuscitative balloon occlusion of the inferior vena cava (REBOVC) to abate massive hemorrhage in retrohepatic vena cava injuries. J Trauma Acute Care Surg 83: 1041-1046. [Crossref]
- Watarida S, Nishi T, Furukawa A, Shiraishi S, Kitano H (2002) Fenestrated stent-graft for traumatic juxtahepatic inferior vena cava injury. J Endovasc Ther 9: 134-137. [Crossref]
