Sudden Cardiac Arrest as the First Manifestation of Takayasu Arteritis
A B S T R A C T
Management of out-of-hospital cardiac arrest (OHCA) remains challenging, particularly in young patients. Takayasu arteritis is a rare large-vessel vasculitis relatively. Coronary involvement has been previously described; we provided the first intracoronary images by OCT. We report the first case of OHCA with shockable rhythm revealing chronic total occlusion of the left main in a 41-year-old lady. The coronary anomaly made it possible to diagnose the vasculitis and to treat it by corticosteroid and immunosuppressive treatment. Vasculitis should be evoked in atypical coronary syndrome in young patients. A collaborative multidisciplinary approach permits optimal care for this complex patient.
Keywords
Coronary artery disease, coronary artery imaging, inflammation, systemic, resuscitation, women heart disease
Case Report
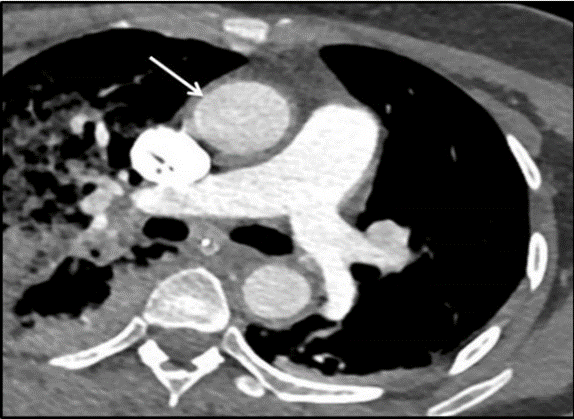
A 41-year-old Asian woman was presented with out-of-hospital cardiac arrest. As she was in a musical concert, she presented a sudden cardiac arrest (SCA), she had immediate chest compression by attending first-aid workers, with a no-flow of less than 2 minutes. Spontaneous circulation was restored after 4 minutes of cardiopulmonary resuscitation and 2 electric shocks. Hemodynamics was stable with no need for inotropic support and electrocardiogram showed sinus tachycardia without repolarization abnormalities. At hospital admission, the scan eliminated recent intracerebral bleeding and pulmonary embolism. Then a coronary angiogram revealed a chronic total occlusion of the ostial left main trunk with complete collateralization by the right coronary artery (Figure 1) (videos in supplemental material). The echocardiography showed no impairment in the left and right systolic function. After review, the CT scan showed increased thickness of the aortic wall of the thoracic aorta extended to the arch branches (Figure 2).
The journey in the intensive care unit was uneventful, with an adapted awakening and she was transferred to the coronary care unit on day 3. The analysis confirmed the absence of acute ischaemic etiology with a slight increase in troponin level (peak, 0.7 mg/L; normal, < 0.05 mg/L) and the cardiac magnetic resonance imaging showed diffuse edema only. The inflammatory markers were also normal.
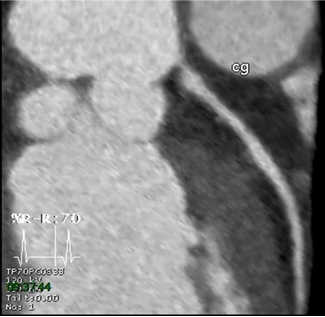
In this context of panarteritis, a comprehensive assessment of aortitis has been completed. All markers were negative. The diagnostic of Takayasu arteritis was retained. A treatment with corticosteroid was given. Installation of a defibrillator and surgical revascularization were decided. The patient refused both despite repeated clear and relevant information about the risks involved. The medical treatment was completed with pulses of corticosteroids followed by tapering corticosteroids associated with anti-interleukin 6 therapy (tocilizumab, 8mg/kg/4 weeks). On 6 months of control, CT scan was unchanged with evidence of a sub-occlusion of the common trunk with collateral flow Rentrop 3 (Figure 3). The patient wore the Life Vest® for 6 months without any recorded rhythmic event. After 10 months of follow-up, the patient was asymptomatic and fine, still refusing surgery and defibrillator.
Figure 1: Coronary angiogram (right view) showing chronic total occlusion of the ostium of the left main stem (arrow) with an ectasic proximal circumflex with a Rentrop 3 collateralization by the right coronary artery.
Figure 2: Initial CT scan showing circumferential thickening of the aorta.
Figure 3: 6 months follow-up CT scan showing the sub-occlusion of the left main stem.
Discussion
Takayasu arteritis is a chronic inflammatory disease of unknown etiology that usually affects young Asian women, involving the aortic arch and the proximal portion of its major branches as well as the coronary and pulmonary arteries [1]. The diagnostic has to be evoked for young patients in front of a typical vascular involvement on imaging, without any other cause of arteritis [2, 3]. If revascularization is needed, it is recommended outside the active inflammatory phase of the disease [4]. Medical treatment is essential and may allow partial regression of vascular lesions [5]. This observation suggests the importance of considering vasculitis as a potential etiology of coronary disease in young patients, in particular young women. A multidisciplinary approach is the key to the care of these complex patients.
Acknowledgements
We would like to thank the cardiologists and MICU physicians and staff.
Funding
None.
Disclosure
None.
Article Info
Article Type
Case ReportPublication history
Received: Thu 12, Nov 2020Accepted: Fri 27, Nov 2020
Published: Thu 10, Dec 2020
Copyright
© 2023 Stephane Manzo-Silberman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.06.02
Author Info
Stephane Manzo-Silberman Alix de Gonneville Martin Nicol Sylvie Meireles Thiziri Simoussi Elise Paven Anne-Claire Desbois David Saadoun Guillaume Lebreton
Corresponding Author
Stephane Manzo-SilbermanDepartment of Cardiology, Lariboisière Hospital, Assistance Publique des Hôpitaux de Paris (AP-HP), Paris University, Paris, France
Figures & Tables

References
- Amsallem M, Henry P, Manzo Silberman S (2014) Optical coherence tomography imaging of Takayasu coronary arteritis. Can J Cardiol 30: 464.e13-464.e14. [Crossref]
- Mekinian ASM, Saadoun D, Gomez L, Comarmond C, Faina O (2017) Management of Takayasu arteritis. Revue du Rhumatisme monographie 84: 229-235.
- Petitpierre S, Bart PA, Leimgruber A, Spertini F, Prior J (2007) Large vessel vasculitis: giant cell arteritis and Takayasu arteritis. Rev Med Suisse 3: 1056-1060, 1062-1063. [Crossref]
- Saadoun D, Lambert M, Mirault T, Resche Rigon M, Koskas F et al. (2012) Retrospective analysis of surgery versus endovascular intervention in Takayasu arteritis: a multicenter experience. Circulation 125: 813-819. [Crossref]
- Yokokawa T, Kunii H, Kaneshiro T, Ichimura S, Yoshihisa A et al. (2019) Regressed coronary ostial stenosis in a young female with Takayasu arteritis: a case report. BMC Cardiovasc Disord 19: 79. [Crossref]
