Journals
Technique of managing a cleft palate in a newborn
A B S T R A C T
Cleft lip and palate are one of the most prevalent congenital anomalies occurring worldwide. The condition is unique in which the management begins right from the time of birth till the second decade, depending upon the situation [1]. Disciplinaries from multiple specialties are involved in the treatment of cleft lip and palate. An array of treatment plan and technique is involved distinctly shows extensive research and studies in this topic of interest.
Keywords
Cleft lip,cleft palate,feeding aid
Introduction
There is an incidence of cleft palate 1 in 700 births [2]. The male: female ratio is 4:3.A male preponderance for clefts has been observed in all major series of patients. Clefts of the palate alone are more common in females with a ratio of 6:4 [3]. The overall incidence of cleft in families is 12.1%. Clefts were associated with syndromes in 63.4% of cases. Left sided clefts are more common than right sided clefts [4].
Etiology
The development of face is coordinated by complex morphogenetic events with rapid proliferative expansion and is thus, highly susceptible to environmental and genetic factors. During the 6th-8th weeks of pregnancy, the shape of the embryo’s head is formed. Five primitive tissue lobes grow, they are the frontonasal prominence, 2 maxillary prominences and 2 mandibular prominences. If these tissues fail to meet, a gap appears, resulting in the formation of cleft. The fusion failure reflects the location and severity of cleft (from a “small fissure” to a “completely malformed face”). Genetic factors contribute to the cleft lip and palate formation. Cleft lip/palate may be present in many different chromosome disorders including Van der Woude syndrome, Stickler’s syndrome, Loeys-Dietz syndrome, Patau syndrome etc [5]. The condition can also occur in an isolated manner without associated with any syndrome. Environmental factors have also been associated with the cause of the clefts. Maternal smoking, maternal alcohol abuse, maternal hypertension, teratogens like anticonvulsants, cocaine, nitrate compounds are some of the documented causes for the formation of cleft lip/palate [6].
Diagnosis
Antenatal ultrasound helps in the diagnosis of cleftlip/palate. Prenatally detected orofacial clefts include diagnosis, karotyping, genetic consultations, psychosocial counseling and neonatal management. In presence of associated major congenital anomalies termination of pregnancy may be considered before the 24th week of pregnancy [7].
Classification of clefts
A number of different classification systems have been proposed over the years. A simple classification based on embryology divides the cleft into 3 categories [8]. 1. Cleft lip & alveolus ( Primary palate) 2. Cleft of hard & soft palate (Secondary palate) 3. Combination of primary & secondary palate. 4. Veau’s classification [9]. 5. Cleft of soft palate 6. Cleft of hard palate & soft palate 7. Complete unilateral clefts of lip, alveolus and palate. 8. Bilateral clefts of lip, alveolus and palate.
Treatment
Cleft lip/palate today is managed successfully by the multidisciplinary cleft team. They are a group of individuals from different specialist backgrounds who work closely together, to bring each specialist’s particular expertise to the patient in the optimum way, thereby enhancing the delivery of the total package. The team includes geneticist, genetic counselor, nurse coordinator, oral & maxillofacial surgeon, orthodontist, otolargyngologist, audiologist, pediatrician, pedodontist, pastic surgeon, prosthodontist, speech pathologist and social worker.
Early intervention
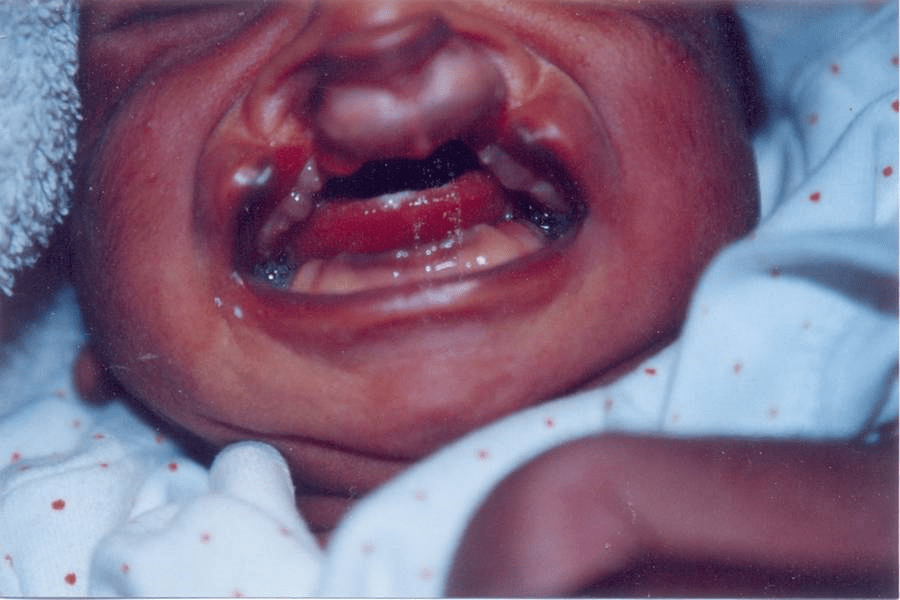
The severity of the cleft and the possibility of other congenital deformities are detected as soon as the child is born (Figure 1). The parents must be made aware of the situation and should be reassured with positive aspects of the child’s appearance. Parents can be comforted by showing preoperative and postoperative photographs of some treated children. Before leaving the hospital, the parents should be able to feed the infant and clean the cleft.
Figure 1: New born
Feeding
Special nursing considerations are required in an infant with a cleft. Maintaining nutrition is of great importance as it’s needed for growth, development and to prepare the infant for the first surgery. Feeding difficulties associated with cleft palate have been documented for many years. In nonsyndromic cases, the underlying problem is thought to be failure to generate sufficient negative intraoral pressure (suction) during feeding. This in turn affects attachment to the breast or artificial nipple and extraction of milk, as well as bolus organization, retention of the bolus in the mouth before swallow initiation, and swallow initiation itself. Sequelae to oral-nasal coupling are reported to include excessive air intake, nasal regurgitation, fatigue, coughing, choking and gagging on fluids, prolonged feeds, and discomfort. Parents may also fear the task of feeding their infant. Literature regarding the feeding of infants with cleft palate is well fed with the potential consequences of feeding difficulties.
Breastfeeding a baby with a cleft palate is challenging. Breast feeding via cup, spoon, and bottle should be promoted in preference to formula feeding. But infants with cleft palate generate negative pressure when sucking and tire easily, ending in incomplete feedings. The mother must position the nipple towards the side of the cleft and support the breast with her finger so as to help the child to grasp the nipple and prevent loss of suction. Hence different approaches are addressed to manage feeding in cleft palate infants. The literature suggests the use of specially designed nipples with enlarged openings increasing the ejection of milk with reduced effort. Soft, premature nipples conform better to the palatal defect than do regular hard nipples. Longer nipples are successful as they can be positioned posterior to the defect. Cross cut nipples allow easier flow of formula. Trial and error method is followed for the selection of the right nipple. The use of squeeze bottle reduces the strain on the infant and allows the parent to squeeze and control the flow of formula into the mouth of the infant. A bulb syringe can also be effectively used as a mode of delivering the formula. Feeding in a semi-upright position decreases the chances of nasal regurgitation. The entire process of feeding requires more time and must be done leisurely, as it takes some time for both the mother and the infant to get adjusted to the technique followed. In case the feeding process extends beyond 45 minutes, then the technique should be reevaluated. Orogastric and nasogastric tubes have been used but the only limitation is that they cannot be used for a prolonged period of time. Surgery completely closes the oronasal communication but the timing for the surgery differs significantly as early as 10-12weeks to well past 12months of age.
Figure 2: Feeding aid
Feeding obturator
The feeding obturator is a prosthetic aid that is designed to obturate the cleft and restore the separation between the oral and nasal cavities (Figure 2). A Feeding appliance, also called as Feeding Aid is defined as “An ancillary prosthesis that closes the oro nasal cavity defect, thus enhancing sucking, swallowing, and maintains the right and left maxillary segment of infants with cleft palates in their proper position until surgery is performed to repair the cleft.” It creates a rigid platform toward which the baby can press the nipple and extract milk. It facilitates feeding, reduces nasal regurgitation, reduces the incidence of choking, and shortens the length of time required for feeding. The obturator also prevents the tongue from entering the defect and interfering with the spontaneous growth of the palatal shelves toward the midline. It also helps to position the tongue in the correct position to perform its functional role in the development of the jaws and contributes to speech development. The obturator reduces the passage of food into the nasopharynx, reducing the incidence of otitis media and nasopharyngeal infections. The literature also shows the feeding obturator to be effective in reducing parents’ frustration over the feeding problems and in relieving anxiety related to the birth of a child with this pathology.
A Prosthodontist may be required to fabricate the obturator. A method for constructing the appliance is presented. The severity of the clefts varies so much that stock trays are not always useful for the impression of the infant's maxillary arch. A preliminary impression is taken by introducing a thermoplastic impression material with the index and middle fingers as the tray. A model is produced from which a custom tray is constructed. The final maxillary impression is taken using an irreversible hydrocolloid with the child in an upright position. An obturator is constructed on the stone model by sprinkling soft autopolymerizing acrylic resin on the palate extending well into the mucobuccal fold area. The cured appliance is trimmed and polished prior to insertion.
Summary
Cleft palate is a congenital deformity that causes a multitude of problems and represents a special challenge to the medical community. Special care is needed for patients with cleft palate. Speech production, feeding, maxillofacial growth, and dentition are just a few important developmental stages that may be affected. The occurrence of a congenital cleft palate greatly impedes the habituation of efficient deglutition of an infant, causing aspiration of fluids in the air passage which may lead to complications like bronchopneumonia and infection of the airway and lungs. Inadequate nourishment due to difficulty in feeding affects the health and acts as an obstacle in the milestones of normal development. Severe nutritional deficiencies further complicate surgical closure at the right time. Prosthodontic treatment has a long and rich history in the care of patients with cleft lip and palate. Because of increased knowledge of craniofacial growth and development and improved surgical and orthodontic treatment, today's cleft patients receive better care and in less time. A feeding obturator given to the infant effectively separates the oral cavity from the nasal cavity and is of great help in feeding till the defect can be surgically repaired. It plays a major role in shortening the time of breast feeding and increasing the amount of food intake and, thus, for the normal growth and development of newborn infants with isolated palate cleft.
Conflicts of interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 05, Apr 2019Accepted: Tue 30, Apr 2019
Published: Wed 10, Jul 2019
Copyright
© 2023 S.C. Ahila. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2019.02.04
Author Info
Corresponding Author
S.C. AhilaReader, Department of Prosthodontics,SRM Dental College,Ramapuram
Figures & Tables

References
- Reid J (2004) A review of feeding interventions for infants with cleft palate. Cleft Palate Craniofac J 41: 268-278. [Crossref]
- World health organization: Global registry and database on craniofacial anomalies. in: organization, W.H. (Ed.) Report of a WHO Registry meeting on craniofacial anomalies. Geneva, Switzerland, 2003.
- San DT, Joseph LBM, Mani M (2007) Statistical analysis of 750 cleft lip and cleft palates. Indian J Plastic Surg 40: 70-74.
- Yoshikazu Nagase, Nagato Natsume, Tomoki Kato, Toko Hayakawa (2010) Epidemiological Analysis of Cleft Lip and/or Palate by Cleft Pattern. J Maxillofac Oral Surg 9: 389-395. [Crossref]
- Kanno K, Suzuki Y, Yamada A, Aoki Y, Kure S et al. (2004) Association between nonsyndromic cleft lip with or without cleft palate and the glutamic acid decarboxylase 67 gene in the Japanese population. Am J Med Genet A 127A: 11-16. [Crossref]
- Bertis B.Little.Drugs, pregnancy (2006) A hand book. Oxford University press P 1-385.
- Garne E, Khoshnood B, Loane M, Boyd P, Dolk H (2010) Termination of pregnancy for fetal anomaly after 23 weeks of gestation: a European register-based study. BJOG 117: 660-666 [Crossref]
- Sperber G H. New York: Oxford University Press (2002). Formation of the primary palate and palatogenesis: closure of the secondary palate; 5-24.
- Veau V Paris: Masson & Cie (1931). Division Palatine.


