The Older Patients and the Epidemiological Change after COVID-19 Pandemic. The Simplicity of the Complexity Management and the Personalization in Cancer Care
A B S T R A C T
The SARS-CoV-2 pandemic has led us to imagine the current scenario as something terrible, disastrous, but temporary. However, history teaches us that an event of this magnitude can only evolve towards “new” normality, a new equilibrium, but it will only be reached through a transition that will last over the years. In this scenario, the term “frailty”, which is known to few, has become common. The need for healthcare that, alongside high specialization, focuses on the complexity of the individual is increasingly intense. Geriatric oncology probably represents the clearest example of how much the current scenario has impacted the health and social fields, as it involves frail adults with cancer. How to draw the future?
Keywords
Older patient, geriatric oncology, complexity management, COVID-19, SARS-CoV-2
Introduction
Since December 2019, the world was involved in an unprecedented global pandemic, coronavirus disease 2019 (COVID-19), caused by a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1-3]. Every country to cope with this emergency has adopted stringent measures to contain SARS-CoV-2 through rapid identification-campaign, obligatory use of facemasks, and isolation of all infected individuals. Many countries have experienced shorter or longer periods of lockdown with significant impacts on society, economy, and lifestyles. Restaurants have been closed, physical activity and educations have been discontinued, venues have been shutting down, and events have been banned. These changes indeed have led to many short-term modifications, but many will determine in the future.
Historically, every significant event has led to changes in the short and long term, even after many years. With the introduction of the atomic bomb, World War II forever changed the balance between nations and unprecedented technological boost. In the post-war period, the restart desire gave birth to the economic boom. Economic boom associated with international migration and increased life expectancy resulted in an extraordinary population increase in developed countries and epidemiological change is referred to as the “baby boom” [4]. Finally, people born in that period, the so-called “baby boomers,” getting older several years later, caused further change resulting in a kind of “silver tsunami” [5]. Baby boomers have been economically and socially different from earlier generations. They have experienced several revolutionary events which have influenced their ways to age. They have been the first generation to have life-extending immunizations, life-saving antibiotics, job opportunities, and education levels not experienced before [6]. The aging of this population group has caused a significant change in health systems with an ever-increasing demand for services and levels of assistance and care appropriated to the high lifestyle they have lived. These same people found themselves facing one of the biggest challenges ever, just when they would be ready to retire in that quiet and comfortable life, they had hoped for them at the sunset of their existence. As a new disease and a new global health issue, COVID-19 is understandable that its emergence and spread caused anxiety and fear among the older population.
The Epidemiological Change after COVID-19 Pandemic
It was proven that the population, including older adults, was generally more susceptible and that older patients had a high rate of infection and mortality [7]. In the world, 3,359,138 people died [8]. (Data from John Hopkins Coronavirus Resource Center, 15.05.2021) Another aspect to consider concerns affected people who have recovered from COVID-19, whose long-term effects have not yet been fully elucidated. Most people recover completely within few weeks. Even those who had mild forms of the disease continue to experience symptoms after their initial admission (post-COVID-19 syndrome or long COVID-19). We know, for example, after a few months of follow-up, that many patients still reported fatigue, dyspnea, joint pain, and chest pain [9]. Probably there will be a future high risk of infections, long-term breathing problems up to respiratory failure, heart complications, neurological syndromes (like stroke, seizures, and Guillain-Barre or an increased risk of developing the neurodegenerative disease), and who knows what else (Table 1 & Figure 1) [10-13].
Table 1: Direct and
indirect consequences of COVID-19.
|
↑ number of deaths |
|
↑ respiratory complications |
|
↑ cardiovascular disease |
|
↑ neurological problems |
|
↑ advanced oncological disease |
|
↑ acute disease |
|
↑ social isolation |
|
↑ mood alterations |
|
↑ neurodegenerative disorder |
|
↑ sarcopenia |
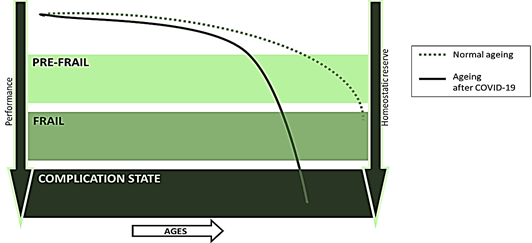
Figure 1: The new aging trajectory of the older patients after COVID-19.
I Will these conditions lead to an increase in comorbidities in the following older patients?
An emerging unaddressed problem not addressed concerns all people not directly affected by SARS-CoV-2 but who have nevertheless suffered the indirect effects of this pandemic. There is a risk that these silent problems will become stunning issues to be addressed in the next future. Starting with the most visible ones, one of the big problems that we will have to and that perhaps we have been already facing is the delay in diagnosing and managing oncological diseases, thus losing the best allies in oncology: the time factor. Many patients have not had the opportunity to adhere to the established outpatients’ controls during the lockdown period, and they instill fear of entering the hospitals [14].
II How will the prognosis of these patients change?
In recent years, thanks to periodic checks, perhaps with excessive medicalization in some cases, many diseases had been managed to become chronic, achieving an increase in the average life span. In the last years, this system built over the years has failed, making it impossible for patients to adhere to screening programmes, carry out outpatient visits, and perform blood and radiological tests.
III What will be the cost? How will the life expectancy of these subjects change?
We will have to expect repercussions not only in the oncology field. In the coming years, we may see an increase cardiovascular diseases, consequences related to diabetes in a landscape of diagnosis no longer in an early stage but in a phase in which treatment will be strictly necessary. This climate of fear and the global lockdown has also turned upside down human relationships, significantly worsening the pre-existing conditions of social isolation and creating new ones. The entire population has been experiencing the mourning of their deceased loved ones and a lifestyle that we will hardly have back precisely as before. The isolation of these months has generated a very harmful hypo-sociality for everyone. The older people died alone, the adults had to change their way of working, the young people had to postpone dreams, renounce training, and the children had found themselves dealing with a world overwhelmed by a tense change [15]. Social isolation has caused a decrease and or alterations in the mood of patients, especially in older patients, with an increase that we have already started to see in our clinics and that could be destined to increase [16, 17]. The fear of contagion has turned into anxiety in all its nuances: hypochondria, agoraphobia, claustrophobia, misanthropic.
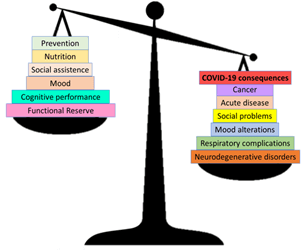
Another significant consequence of this historical period has also concerned the functional performance of patients, both cognitive and physical. With the reduction of social interactions, the increase of depression, and the decrease of activities and stimuli, there is the risk that will increase in cases of cognitive impairment in this climate of limitations and fear [18, 19]. The reduced possibility of leaving the house and exercising, on the other hand, will be responsible for a significant decrease in physical performance and worsening of outcomes in many areas [20-22]. Thus, what is the next COVID-19? We do not know, but certainly, we will live in a changing society, both for the number of deaths and for the long-term direct and indirect complications of the COVID-19. If the dead were many, many more are the people who will have future consequences (Figure 2).
Figure 2: The weight of the COVID-19 consequences in the delicate balance of frail older patients.
Conclusion
The concept of frailty as the pandemic has taught us eludes the magnificence of ultra-specialization to bring us back to the simplicity of seeing man and disease as a whole with its complexity. If we still considered diseases as belonging to single organs and managed as in single chapters or boxes, we would be pursuing the error that led us to have expensive but ineffective health systems. The specialized organization we have is fundamental, but as in cancer management, the personalization of care is often confused with target therapy, leading to complex management of the elderly cancer patient. We must rethink cancer management in a more holistic scenario with a new type of frail patients and their morbidities at the center and not only cancer.
Article Info
Article Type
Review ArticlePublication history
Received: Mon 17, May 2021Accepted: Tue 08, Jun 2021
Published: Tue 30, Aug 2022
Copyright
© 2023 Giuseppe Colloca. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ACO.2021.01.01
Author Info
A. Bellieni D. Fusco F. Benvenuto S. Bracci E. Villani B. Di Capua F. Marazzi L. Tagliaferri L. Balducci S. Monfardini V. Valentini Giuseppe Colloca
Corresponding Author
Giuseppe CollocaFondazione Policlinico Universitario A Gemelli IRCCS, Rome, Italy
Figures & Tables
Table 1: Direct and
indirect consequences of COVID-19.
|
↑ number of deaths |
|
↑ respiratory complications |
|
↑ cardiovascular disease |
|
↑ neurological problems |
|
↑ advanced oncological disease |
|
↑ acute disease |
|
↑ social isolation |
|
↑ mood alterations |
|
↑ neurodegenerative disorder |
|
↑ sarcopenia |
References
1. World Health
Organization (2020) Novel Coronavirus (2019-nCoV): situation report, 22.
2. Zhu N, Zhang D,
Wang W, Li X, Yang B et al. (2020) A Novel Coronavirus from Patients with
Pneumonia in China, 2019. N Engl J Med 382: 727-733. [Crossref]
3. Balducci L, Colloca
G (2020) Natural disaster and rationing of care. J Geriatr Oncol 11:
750-752. [Crossref]
4. Hugo G (2013) The
changing demographics of Australia over the last 30 years. Australas J
Ageing 32: 18-27. [Crossref]
5. Bluethmann SM,
Mariotto AB, Rowland JH (2016) Anticipating the “Silver Tsunami”: Prevalence
Trajectories and Comorbidity Burden among Older Cancer Survivors in the United
States. Cancer Epidemiol Biomarkers Prev 25: 1029-1036. [Crossref]
6. Buckley J, Tucker
G, Hugo G, Wittert G, Adams RJ et al. (2013) The Australian baby boomer
population - factors influencing changes to health-related quality of life over
time. J Aging Health 25: 29-55. [Crossref]
7. Yang X, Yu Y, Xu J,
Shu H, Xia J et al. (2020) Clinical course and outcomes of critically ill
patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered,
retrospective, observational study. Lancet Respir Med 8: 475-481. [Crossref]
8. John Hopkins
University & Medicine. COVID-19 Map - Johns Hopkins Coronavirus Resource
Center.
9. Carfì A, Bernabei
R, Landi F, Gemelli Against COVID-19 Post-Acute Care Study Group (2020)
Persistent Symptoms in Patients After Acute COVID-19. JAMA 324: 603-605.
[Crossref]
10. Ayoubkhani D,
Khunti K, Nafilyan V, Maddox T, Humberstone B et al. (2021) Post-covid syndrome
in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ
372: n693. [Crossref]
11. Varatharaj A,
Thomas N, Ellul MA, Davies NWS, Pollak TA et al. (2020) Neurological and
neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide
surveillance study. Lancet Psychiatry 7: 875-882. [Crossref]
12. Long B, Brady WJ,
Koyfman A, Gottlieb M (2020) Cardiovascular complications in COVID-19. Am J
Emerg Med 38: 1504-1507. [Crossref]
13. Fraser E (2020)
Long term respiratory complications of covid-19. BMJ 370: m3001. [Crossref]
14. Zubiri L, Rosovsky
RP, Mooradian MJ, Piper Vallillo AJ, Gainor JF et al. (2021) Temporal trends in
Inpatient Oncology Census Before and During the COVID-19 Pandemic and Rates of
Nosocomial COVID-19 Among Patients with Cancer at a Large Academic Center. Oncologist.
[Crossref]
15. Tang F, Liang J,
Zhang H, Kelifa MM, He Q et al. (2021) COVID-19 related depression and anxiety
among quarantined respondents. Psychol Health 36: 164-178. [Crossref]
16. Bueno Notivol J, Gracia García P, Olaya B, Lasheras I, López Antón R et al.
(2021)
Prevalence of depression during the COVID-19 outbreak: A meta-analysis of
community-based studies. Int J Clin Health Psychol 21: 100196. [Crossref]
17. Delmastro M,
Zamariola G (2020) Depressive symptoms in response to COVID-19 and lockdown: a
cross-sectional study on the Italian population. Sci Rep 10: 22457. [Crossref]
18. Manca R, De Marco
M, Venneri A (2020) The Impact of COVID-19 Infection and Enforced Prolonged
Social Isolation on Neuropsychiatric Symptoms in Older Adults With and Without
Dementia: A Review. Front Psychiatry 11: 585540. [Crossref]
19. Cagnin A, Di Lorenzo R, Marra C, Bonanni L, Cupidi C et al. (2020) Behavioral
and Psychological Effects of Coronavirus Disease-19 Quarantine in Patients With
Dementia. Front Psychiatry 11: 578015. [Crossref]
20. Landi F, Calvani R, Cesari M, Tosato M, Martone AM et al. (2015) Sarcopenia
as the Biological Substrate of Physical Frailty. Clin Geriatr Med 31:
367-374. [Crossref]
21. Argilés JM, Campos N, Lopez Pedrosa JM, Rueda R, Rodriguez Mañas L (2016) Skeletal Muscle Regulates Metabolism via Interorgan Crosstalk: Roles in Health and Disease. J Am Med Dir Assoc 17: 789-796. [Crossref]
22. Colloca G , Di Capua B, Bellieni A, Cesari M, Marzetti E et al. (2019) Erratum to ‘Muscoloskeletal aging, sarcopenia and cancer’ [Journal of Geriatric Oncology, Volume 10, Issue 3, May 2019, Pages 504-509]. J Geriatr Oncol 10: 839. [Crossref]
