The Role of Rehabilitation in Peripheral Paralysis of the Facial Nerve: A Case Report of a Patient Treated with a Neuro-Cognitive Approach
A B S T R A C T
Peripheral paralysis of the facial nerve is a pathology that, although not involves any risks for the patient's life, significantly affects not only motor, but also communicative, psychological, and social aspects, having an important impact on the quality of life. The most widely used therapeutic proposals do not always respond to the need to intervene on all the functional components related to the facial nerve, but to prevent and treat complications. The neuro-cognitive proposal, although not found in the literature or in the biomedical databases, takes into account the motor, communicative, verbal and non-verbal functions related to facial mimic, as well as the cognitive-exploratory function of some districts of the face and intervenes following the phases of nervous recovery limiting an abnormal reinnervation. The case reported concerns a patient with a paralysis caused by surgical removal of acoustic neuroma (vestibular schwannoma), with grade III on the House-Brackmann scale, seems to be an example of how an approach of this type is constructed in such a way as to follow the various phases of recovery of the peripheral nerve injury, promoting the recovery of the various functions related to the facial. The patient evaluated with the Sunnybrook Facial Grading System (SFGS) went from 21/100 to 92/100 and did not develop synkinesias after about 5 months of treatment. The neuro-cognitive approach would seem to progressively improve the quality of movement. Moreover, being selective with respect to muscle recruitment and inserted in a functional perspective that respects recovery times, it would seem to limit the appearance of pathological sequelae such as synkinesias and spasms.
Introduction
Peripheral paralysis of the facial nerve (PPF) consists of a mono neuritis caused by lesions affecting the nucleus of the VII cranial nerve at the pontine level, or the trunk of the nerve itself during its course [1]. It must be considered that the nucleus of the nerve has anatomical peculiarities that condition the results of any injury to the fibers. It consists of two sub-units: an upper one which provides the innervation of the lower portion of the face receiving fibers from the contralateral corticospinal bundle and a lower one which receives fibers from both the ipsilateral and contralateral cortex, delegated to the innervation of the upper part of the face. As a result, a peripheral lesion of the facial nerve will result in a deficit of the whole ipsilateral half-life at the site of the lesion, which is generally more complex than a central paralysis, which affects only the contralateral lower half-life.
From an epidemiological point of view, peripheral paralysis of the facial nerve is the most frequent pathology of the cranial nerves [2]. It is quite frequent with an incidence that varies between 20 and 30 new cases per year per 100,000 inhabitants [3]. Among these, the prevalent form is Bell's palsy, which represents up to 75% of all those of the facial nerve [4, 5]. From a prognostic point of view, in Bell's Palsy of an idiopathic nature, about 30% of patients do not have a complete recovery and sometimes unpleasant complications appear, such as altered synkinesias, contractures, spasms, salivation and tearing. In the secondary forms of tumors and surgery the prognosis depends on the type of tumor or surgery [6, 7].
The peripheral paralysis of the VII cranial nerve, while not involving life-threatening effects, however, heavily influences the way of life of the affected subjects, for the functional, psychological, social and working aspect on which it impacts. Pharmacological treatment based essentially on the use of corticosteroids and antivirals (if viral genesis is suspected) is associated with rehabilitation. The recovery of the motility of the affected half-face is a complex process that cannot be considered only from a biomechanical point of view, but must contemplate multiple related aspects, such as non-verbal communication (mimic), the function associated with chewing and swallowing. There are numerous rehabilitation approaches that are used for this pathology and in the literature, there are various works and some revisions.
Clinical Manifestations
Peripheral paralysis of the facial nerve is defined as a sudden paralysis paresis that involves all the muscle groups of the homolateral half-life to the lesion. It may be accompanied by other symptoms such as: skin pain on the affected side, disorders of various sensitivities, ipsilateral hyperacusis [8]. The most characteristic symptom of damage to the facial nerve is the deficiency of the motor function: the latter can be complete and take the name of paralysis, or partial, and in this case, it is called paresis.
The paralysis of the facial presents a heterogeneous picture that also emerges at rest with asymmetry of the features: most patients have a buccal rhyme deviated towards the healthy side, smoothing of the wrinkles of the affected emilate, "fall" of the lower eyelid and epiphora. The patient will not be able to wink, wrinkle his forehead or eyebrows, curl his nose, smile, show his teeth symmetrically, whistle, blow, swell his cheeks, send a kiss, he will also have difficulty drinking and eating, consequently it will have repercussions on the plane of language and swallowing. All these inconveniences translate into a sharp reduction in social life and the appearance of phenomena such as depression and anxiety.
From a static examination of the face, the following symptoms are highlighted:
i. Sliding of the buccal rim.
ii. Asymmetry of the features with smoothing of frontal wrinkles, the intersection of the eyebrow and the nasolabial sulcus.
iii. Eyelid drops from the affected side.
iv. Sliding of the back of the hemilingual from the affected side, visible if the patient is asked to hunt it.
v. Epiphora: a clinical ocular sign that consists in the extravasation of tears from the conjunctival sac and possible fall on the cheek.
vi. Sometimes loss of saliva on the affected side.
A dynamic facial examination shows that the patient cannot:
i. Tighten eyelids and mouth.
ii. Wrinkle the forehead, raise and frown due to deficit of the frontal muscle and corrugator of the eyebrow.
iii. Inflate the cheek and retain air and liquids.
iv. Chew properly, for buccinator and orbicular muscle deficit of the mouth.
v. Whistle and blow effectively.
vi. Lagophthalmos: the incomplete closure of the eyelid rim. If not treated properly there is the possibility of the appearance of an exposure keratitis.
These functions will also be compromised due to the fact that, despite motor deficits being the signs and symptoms par excellence of PPF, facial fibers not only act as a somatomotor components and, consequently, tactile deficits are often associated with the deficit of voluntary muscles and taste. To make the picture even more complex is the frequent manifestation of some typical signs such as the Bell sign, which manifests itself at the request to close the eyelid from the injured side, with the upward rotation of the eyeball and the phenomenon of "tears from crocodile”, due to an incorrect axonal regeneration of the fibers destined for the submandibular-sublingual ganglion. These go to the spheno-palatine ganglion which innervates the lacrimal glands, and which manifests itself with the appearance of the tear reflex instead of the salivation reflex when eating.
The factors and mechanisms that can condition the course of the disease and therefore the possible possibility of an incomplete recovery are still unclear: conflicting opinions emerge regarding age, while a more uniform opinion may be found on the link between the degree of nerve injury and the chances of recovery: patients with degeneration greater than 85% on electroneurography show a recovery rate significantly lower and slower [9, 10]. It should also be considered that in the case of axonotmesis, movement begins only after nerve regeneration [4]. Concerning complications, the most feared and frequent is the development of syncinesias: it has been seen that the probability of occurrence of the latter in patients with incomplete recovery can reach up to 42% [11].
Synkinesia is an abnormal associated involuntary facial movement, such as closing the eyes during a smile (oro-ocular synkinesia) or mouth movement during the blink of the eyelids (oculo-oral synkinesia), presumably due to the incorrect innervation that develops during the process of reinnervation of the facial muscles [12, 13]. The reflection on how much this complication can affect the psychological-relational aspect of the patients is immediate, at the same time we must also evaluate other implications of this pathology: in the most serious cases, in fact, the facial muscles being so frequently contracted tend to shorten and lose elasticity. This will not only make recovery more complex but will be further cause for discomfort for the patient who will experience a prolonged and unpleasant sensation of stiffness in the affected cheek.
Despite being the most frequent and documented, synkinesia is not the only complication of PPF: in fact, patients can experience altered spasms, salivation and tearing and therefore to phenomena such as the crocodile tears syndrome or epiphora [14]. After a nerve injury, if this does not affect the cell body with cell death but the axon, if the extracellular environment favors it, this can regenerate and re-establish contacts with the target cells, with consequent functional recovery.
Moreover, various sprouting phenomena occur, stimulated by muscle denervation. Lotter and Quinci therefore argue that muscle not only represents the target of neurogenic damage, but also the starting point of the processes of nerve regeneration [15]. Denervated muscle fibers undergo an atrophic process and, due to the insufficient supply of Na+, due to axonoplasmic blockade, diffuse depolarization occurs. These conditions will favor the increase in sensitivity to acetylcholine, which will extend to the entire muscle surface and no longer to the neuromuscular junctions only. The inactivity of the muscle and the extension of the acetylcholine-sensitive surface, associated with the production of growth factors following the injury, stimulate the collateral sprouting processes: therefore, collateral compensatory pathways are created towards the denervated muscle fibers allowing their re-innervation and restore function. Within the 15 days following the injury, regenerative processes begin through two main routes: direct route (budding) in which we witness the birth of fibrils from the healthy stump that will reach the distal one, and indirect route (collateral sprouting) in which we witness the innervation of denervated muscle fibers by a healthy nerve. Miehlke, Stennert and Chilla (1979) have identified recovery phases after an anastomosis or nervous implant [16].
In the first phase, the initial delay phase, the axons undergoing regeneration appear in the proximal trunk of the peripheral nerve segment. In the second phase, the maturation phase, the axons undergo regeneration. In the third phase, the final delay phase, the axons reach the motor plates and effective recovery of function occurs. The authors obviously highlight that there are factors that influence the speed of regeneration, such as the nature of the lesion, the type and size of the injured nerve fiber and the age of the patient. They also argue that, for this to happen, must pass at least three months. It is interesting to note that in the neurocognitive proposal used for this clinical case, the same terminology is used to define the three successive stages of rehabilitation, making them correspond to those of the clinical evolution of the pathology.
Rehabilitative Evaluation
In patients suffering from peripheral paralysis of the facial nerve, physiotherapy aims to facilitate and to promote the gradual recovery and optimization of the use of mimic muscles and the functions connected to them, allowing the return to a better functional dimension and psychosocial. Each therapeutic act always starts from an adequate evaluation that allows to recognize the patient's needs and that allows the comparison of the outcomes following rehabilitation treatment. The evaluation of facial nerve palsy mainly focuses on the clinic: after carrying out an accurate medical history, observation of the patient and administration of evaluation scales are essential. The different scales can be supported by attached photos and videos, thus obtaining a more complete picture of the clinical case.
The assessment should be performed no earlier than 3-5 days from the onset of the paralysis and will then be repeated to monitor the course of the disease. It must be completed with an analysis of functional impairment, also investigating any precautions that the patient must take to protect the eye from complications. As regards the difficulties of chewing, the tongue can be compromised and sometimes dysfunctions also occur in the submandibular and sublingual glands, which secrete saliva, therefore food residues may stagnate in the oral cavity. It is important to also investigate how the patient drinks, whether he needs aids or not. Many of these investigations are predicted by the scales of peripheral paralysis of the facial nerve. In fact, many of them were developed over the years with the aim of objectively documenting the relative functions of the facial nerve, monitoring recovery and facilitating communication between professionals.
Among the various PPF rating scales the best known is House Brackmann (HB), in which there are six degrees of severity of the pathology. The different stages are differentiated not only on the basis of the residual functionality of the musculature of the affected half-life and facial symmetry, but also on the basis of the appearance or otherwise of complications such as contractures or synkinesias.
I House-Brackmann Classification
Grade I. Normal facial movements. No synkinesias.
Grade II. Slight facial asymmetry.
Grade III. Obvious facial asymmetry. Closing the eye still possible. Bell phenomenon present.
Grade IV. Obvious paralysis. Synkinesias.
Grade V. Marked asymmetry. Inability to close the eye.
Grade VI. No tone. Complete paralysis.
The limits attributable to HB are not few: the system is of considerable subjectivity in the assessment does not allow assessments of different degrees depending on the district of the face considered [17]. The scale is therefore not very sensitive to small variations.
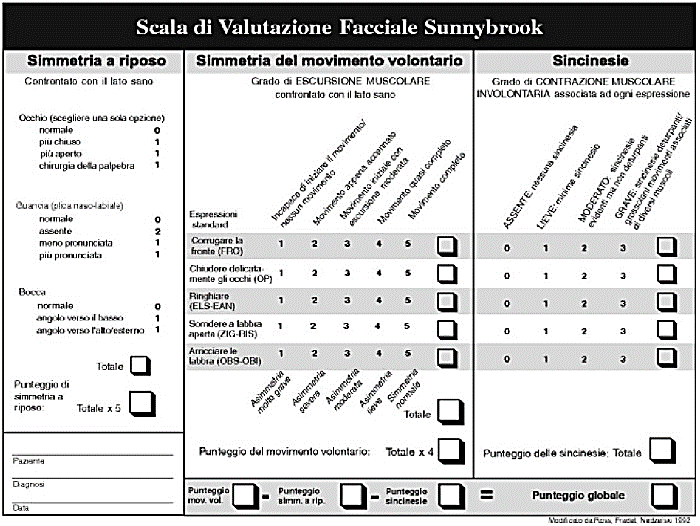
II The Facial Grading System
The Facial Grading System or the Sunnybrook Facial Grading System (SFGS), introduced in 1996, Ross et al. is a scale used to evaluate facial function [18]. This system has been shown to have high internal consistency, high repeatability and good sensitivity to clinical changes. In addition, it showed good correlation with other classification systems in use, including the House-Brackmanne and Yanagara scales.
The Sunnybrook Scale assigns a score from 0 (complete paralysis) to 100 (normal function), allowing the evaluation of the patient both at rest and during voluntary movement and the analysis of any synkinesias that have developed. The assessment is always carried out through a comparison with the healthy side and a differentiation of the different districts of the half-life considered. In 2013 the Italian version of this scale was published by the group of Chiara Pavese and the authors declare that the Italian version of the SFGS has excellent internal consistency and reproducibility, comparable to the original one [2].
Also, in a 2015 review the authors recommend the widespread adoption of the Sunnybrook scale as the current standard in reporting the results of facial nerve disorders [19]. The Facial Disability Index (FDI) evaluates the feedback that the pathology has in the patient's daily life. The complications or the excursions of the single movements are not analyzed, but the alterations of the ADL, relational and psychological that follow. The FDI therefore assesses the patient's difficulties in activities such as nutrition, personal care, communication, but also the quality of sleep and the patient's psychological conditions. There is an Italian version of this scale validated in 2014 by the group of Chiara Pavese [2].
Functional Systems Related to the Facial
The facial nerve and the muscles innervated by it constitute a functional system in itself, in which some functions are shared with other cranial nerves; for example, tactile sensitivity of the auricular basin but probably also of the face (in association with the trigeminal), proprioceptive of the face (in association with the trigeminal) and gustatory (calices of the front 2/3 of the tongue); regulates the excito-secretory function for the submandibular and submaxillary glands, the nasal and palatine mucosa, and the lacrimal gland, contributes to the regulation of tympanic tension, accommodation and chewing. It is involved in verbal and non-verbal-mimic communication and for this reason rehabilitation must be aimed at multiple systems that cooperate with each other. Following the publication of recent studies on emotions, it emerged that facial mimic is regulated by the limbic and cortical systems: two distinct ways which, however, act synergistically, belonging to the same system [20].
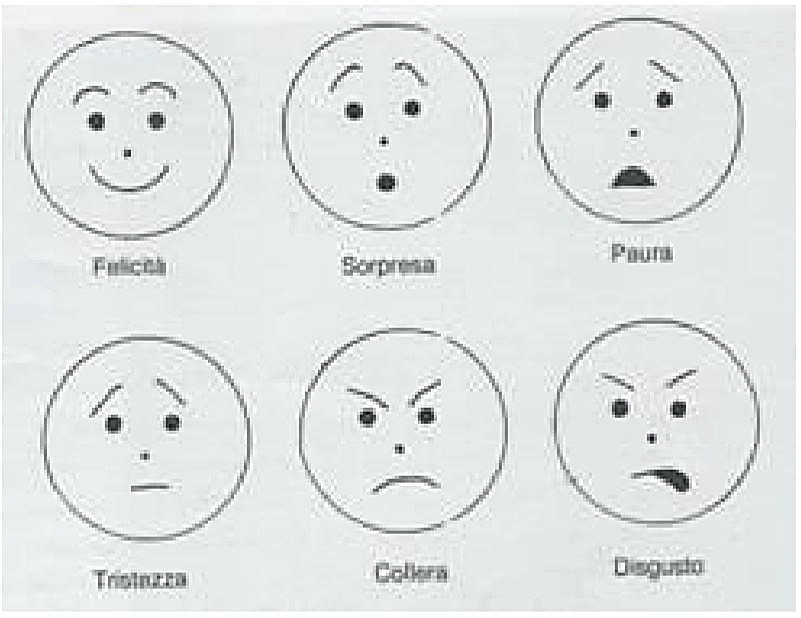
The facial mimic is regulated by two ways that guarantee the innervation to the nucleus of the VII cranial nerve: the voluntary expressions use the circuit of the cortico-bulbar way, the involuntary ones (typical of emotions) instead use the extrapyramidal and limbic one [21]. Consequently, the interruption of one way is a sure cause of the ineffectiveness of the other. The paralysis of the facial nerve compromises the part of the body engaged in the transmission of communicative signals in interpersonal relationships, such as moods, emotions. The rehabilitator cannot overlook these considerations since the treatment must be aimed at overall rehabilitation. As already mentioned, paralysis of the VII cranial nerve affects multiple functional systems. They are:
i. Communication (verbal and non-verbal);
ii. Vision (is facilitated by periorbital movements regarding accommodation, blinking);
iii. Hearing (facilitated by the regulation of tympanic tension);
iv. Smell (facilitated by the opening of the nostrils);
v. Digestion (salivation, chewing, sucking)
Furthermore, paralysis also leads to deficits in various sensory and perceptual modalities; psychological dynamics that slow down recovery may also occur. The innovative hypothesis of a type of organization and control based on functional systems was inevitably followed by a new concept of recovery which, according to neuro cognitivists, is a learning modality: in this systemic perspective, movement is understood as knowledge and as a means of interaction between the external and internal world. Movement is therefore one of the final objectives of rehabilitation treatment and not an exercise to be proposed.
Rehabilitation According to the Cognitive Neuro Approach
To promote patient recovery, it is therefore essential to know the cognitive processes aimed at learning and interacting with the outside world: movement (intended as action with a specific purpose), perception, memory, attention, sight, language and ability to solve the problems. Another aspect that the therapist must necessarily take into account is the importance of the verbal, non-verbal communication function and of the cognitive function (through the tactile and kinesthetic sensitivity of the face), in the functional system of the VII cranial nerve [1]. On these assumptions is based the proposal of the neurocognitive rehabilitation method of Professor Perfetti and collaborators.
In addition, the previously reported hypotheses have led neuro cognitivists and other authors to criticize other therapeutic approaches:
i. Electrostimulation would seem to produce a decrease in cholinergic sensitivity and inhibit neuronal sprouting, as blocking neuromuscular transmission could increase the number of neurons that survive thanks to the neurotrophic factor. Conversely, direct muscle stimulation appears to favor neuronal death. In addition, stimulation is not limited to the individual muscle fibers involved but is widespread and could also involve the surrounding fibers, including the sensitive and neurodegenerative ones, on which the effect is unknown. Some authors recommend electrotherapy with long pulses to limit excessive and rapid collateral innervation [1]. Animal studies have however shown that electrostimulation leads to inhibition of reinnervation and inhibition of sprouting [22, 23]. A systematic review of 2017 on this topic concludes that there is no evidence to support the use of electrostimulation and in a 2012 Cochrane review, the authors conclude that electrostimulation does not produces no benefit, while claiming that as far as facial exercises are concerned, even if the relative studies were of low quality, they would seem to be able to help improve facial function mainly for people with moderate paralysis, in chronic and more severe cases they can reduce the recovery time [4, 24].
ii. Kinesitherapy according to proprioceptive neuromuscular facilitations (Kabat) pays particular attention to voluntary movement but not to that generated by emotions, through the limbic system and therefore would neglect the approach from the perspective of a functional system so important for sensorimotor recovery [1].
iii. Mime therapy consists in the reproduction of stereotyped expressions not inserted in a communicative context, which do not assume any meaning for the central nervous system and therefore are not activated by the limbic system, but by the cortico-bulbar system [1]. The authors of the review Peripheral Facial Nerve Palsy: How Effective Is Rehabilitation find that adaptations induced by the rehabilitation of facial nerve injuries occur mainly in the cortex [10]. In this regard, report the results of two studies, Diels HJ's review "Facial paralysis: is there a role for a therapist ?! 2001 and the 1997 study "Cortical reorganization in patients with facial palsy" [25, 26].
Analyzing these studies, the authors conclude that the changes that occur in the cortex are possible due to the plasticity of the brain, that is, its ability to alter its organization based on stimuli and that in case of facial paralysis after a month, due to of deafferentation, part of the sensory representation of the face can be occupied by the representation of the hand. The authors therefore note that rehabilitation can guide this plasticity by inducing a change in the patterns represented in the cortex. It therefore seems that all the conditions are present for intervening with a neurocognitive rehabilitation method, according to the approach of Carlo Perfetti and collaborators, a revolutionary approach that has applied the scientific discoveries of the last decades on brain functions and their development to the world of rehabilitation and their recovery after an injury. From a research on biomedical databases, no publications were found that deal with neurocognitive rehabilitation according to the approach of Professor Carlo Perfetti. On PubMed the only work that uses a neurocognitive approach is based on the use of motor imagery and mirror therapy [27].
An article entitled "Emotional training in peripheral paralysis of the facial nerve" has been published on Minerva Riabilitativa in 2018 [28]. The proposed rehabilitation approach for the proposed study is based on the neurocognitive method. The results obtained by the 39 patients are encouraging, although not uniformly positive.
Therefore, to deepen the neurocognitive approach according to Perfetti, it was necessary to refer to the magazines and books published by neurocognitive rehabilitators [1, 15, 29-31]. The hypothesis behind the cognitive theory is that through the activation of these fundamental processes to allow man to relate to the world to know it, the CNS can achieve a perfecting of this ability to interact both in normal conditions (learning) and in pathological conditions (recovery). Recovery is a method of acquisition, in this systemic perspective, movement is understood as knowledge and as a means of interaction between the external and internal world. The body is a somesthesic receptor surface capable, through its fragmentation, of providing the Central Nervous System with the information needed in a given situation for the purpose of knowledge and assignment of meaning to the surrounding world [1]. It is necessary to pay attention to what cognitive processes are useful for the subject to know and learn. Those useful to enter into relationship with the surrounding world are:
i. Movement (intended as an action with a certain purpose)
ii. Perception
iii. Memory
iv. Caution
v. Language
vi. Ability to solve problems
Each rehabilitator has tools through which he teaches the patient motor strategies to be implemented when the pathology occurs and then to be learned for functional recovery. The cognitive problem: the mode of interaction with the patient must be consistently represented by the request to activate cognitive processes in a programmed manner.
I The Perceptual Hypothesis
Faced with each problem, the patient must formulate one or more hypotheses which must then be tested. These must relate to the process to which it will be subjected and what will be perceived through interaction with the world carried out with the help of the physiotherapist.
II Mental Processes
Without the activation of cognitive processes, the patient cannot solve the proposed cognitive problem, because he does not elaborate the perceptual hypothesis.
III Motor Image
Represents a way to anticipate and simulate actions. In fact, when the central nervous system produces one or more hypotheses in order to solve a problem, it has the possibility of anticipating its validity through the use of the image. By evoking a correct image, the patient can more easily find a trace that guides him to solve the task. The fundamental problem for the rehabilitator is to teach the patient to produce a true motor and non-visual image [1].
In addition to the motor image, the neurocognitive approach also involves the use of the comparison with the pre-injury action and that performed with the healthy part. In fact, in recent years it has emerged that confrontation is an important mental process for learning, knowledge and the acquisition of awareness [32]. Regarding the peripheral paralysis of the VII cranial nerve, it is necessary to consider some components of the functional system to be rehabilitated such as:
IV The Verbal Communication Function
The production of language through the vowel and consonant phones takes place through the movements of the buccal region and cheeks.
V The Non-Verbal Communication Function
Personalities and emotions are manifestations of the person communicated through the face and mimicry.
VI The Cognitive Function
These occurs through tactile and kinesthetic recognition at the level of the various areas of the face. For example, let’s think for example, of the extraordinary tactile sensitivity of the lips that allows the identification of objects and food brought to the mouth or the ability of the nervous system to know the situation of the districts at all times thanks to proprioception [1]. The lips can even recognize the different shapes (stereoagnosia), the differences in consistency (batiesthesia) and roughness (epicritic tactile sensitivity) of the surfaces that come into contact with the buccal rhyme. The realization of facial expressions is possible thanks to the kinesthetic sensitivity.
According to Ekman (2003), the individual has the possibility of raising the succession of his moods to a conscious level and this essentially occurs through kinesthetic sensitivity [33]. This faculty consists in the ability to recognize the "key points" of the face in the current situation and to know how to compare it with their rest position in order to be able to use them, according to the needs and the context, through an adequate muscular action [1]. The cognitive function gives meaning to facial movements and from them draws elements on the external environment and on one's own organism. Therapeutic exercises are ordered in three successive moments (I, II, III) and follow the patient's clinical evolution.
Exercises Phase I (Initial Delay Phase)
They are aimed at the patient's relaxation, awareness of his face and the possible state of contracture. The patient is required to recognize with closed eyes the characteristics of certain figures, surfaces or movements of segments of the face performed by the therapist. No voluntary contraction is required. The patient must pay only attention to elaborate and verify the perceptive hypothesis. Exercises involving voluntary contraction and indirect mechanical stimulation of the muscles should be avoided.
Exercises Phase II (Final Delay Phase)
After developing an adequate ability to perceive the face in the various components and to control the phenomena associated with exaggerated irradiation, the patient can perform simple movements inherent in the main facial expressions of the emotions. We then move on to more demanding parcel type that involve multiple districts of the face. It is a matter of carrying out voluntary movements for expressive purposes. The cognitive exercises of phase one are also used but the patient will participate actively by recruiting motor units compatibly with his skills.
Exercises Phase III (Functional Recovery Phase)
The patient is put in a position to freely express himself and to invent himself a context in which, through facial expression and dialogue, a communication relationship can be established. He must therefore have developed his own autonomy in the management of the exercises, but the role of the physiotherapist is fundamental for that of intervening as feedback, influencing the patient's emotionality and guiding him in the progression of the activities to be carried out more and more independently [1].
The Clinical Case
The patient in question, a female 44-year-old teacher, after the removal of an acoustic neuroma (vestibular schwannoma) presents the paralysis of the left facial nerve. Evaluation cards with photo and video support were administered at all stages of the treatment.
From direct observation 10 days after her onset, the woman manifests the symptoms of peripheral suffering of the VII cranial nerve of grade III on the House-Brackmann scale. The patient has no frontal wrinkles on the affected side, the eyebrow and left eyelid slightly lowered, evident difficulty in closing the eye (slightly red), Bell's sign is present, it contains liquids in the mouth but cannot move them without leaking , can't blow and kiss. It presents difficulties in pronouncing lip syllables. Deficiency of the tactile and kinesthetic sensitivity of the left half-face. He reports disturbances of the gustatory sensation (bitter taste). When he smiles and shows his teeth, the hypomobility of the affected side and the prevalence of the healthy side are evident.
Given the impossibility of closing the eye, the patient was prescribed by the ophthalmologist to carry out serious and accurate prevention of eye complications, using protective eye drops and some measures such as leaving the house, at least for the first time, with the blindfolded. From the first meeting, the patient immediately showed excellent participation and motivation in rehabilitation treatment according to the neurocognitive approach.
The patient performed the rehabilitation treatment on average 4 times, for the first month and then 3 times a week for about four months.
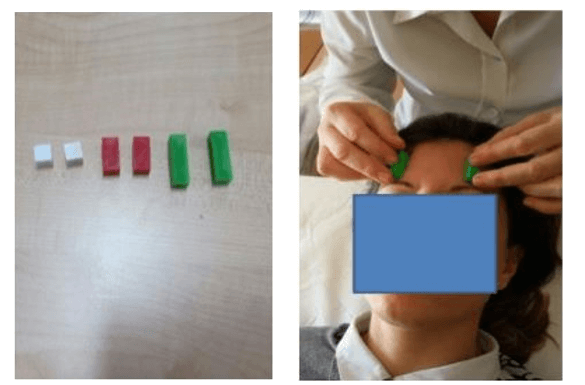
Recognition exercises of size and consistency have been proposed in the various key points of the face including:
i. Recognition of five plastic cuisenaire rods near the midline (forehead, chin area and maxilla).
ii. Recognition of five different surfaces near the midline of the face (forehead, chin area and maxilla).
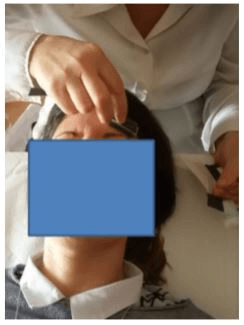
iii. Recognition of sponge pads of 3 -4 different sizes laterally to the eye.
iv. Recognition of shapes on the eye (circle, square, triangle).
v. Recognition of displacements of soft parts of the face.
vi. Recognition of three positions of the closure of the eye using the motor image.
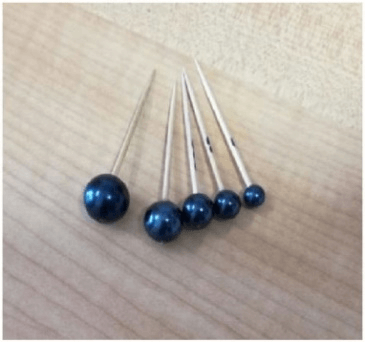
vii. Recognition of size of three dice of different sizes between the lips and in the mouth, between teeth and cheeks.
viii. Recognition of different sizes between the lips.
Two types of comparison were used. The first occurred with the healthy side especially when the patient had difficulty in discrimination, initially proceeding near the midline and gradually moving away from it to facilitate recognition. The second comparison took place with what was perceived in anticipatory terms, also evoking significant sensorimotor images linked to emotional aspects and requesting the patient to bring those sensations back to the movements she was about to feel. From a first evaluation with the FGS, 20 days after the onset, the patient scored a score of 21 and already showed some albeit minimal improvements, such as the recovery of sensitivity near the midline of the face. It still had the Bell phenomenon, the angle of the mouth stretched downwards and the less pronounced nasolabial sulcus. The frontal wrinkles were absent, but he managed to close his eye even if not completely, he mentioned movements such as curling his lips, smiling and blowing. He still could not move the food with his tongue, nor could he pronounce a few words like mom, baby food, dad, grapes. There was no synkinesia present.
With Phase 2, other exercises were proposed to introduce some voluntary movement by the patient, including:
i. recognition of dimensions and shapes far from the midline;
ii. recognition of expansion between the lips.
Spheres of different sizes were used for the closing movement of the lips, which the patient had to explore with more and more active recognition methods.
Furthermore, expansion recognition exercises of different consistency (from the softest to the hardest, up to five consistencies) between the lips have been proposed.
In this second phase, the II-degree exercises were the protagonists (through voluntary movement with expressive purposes), through the recognition and imitation of patterns representing facial expressions (those of Ekman and subsequently with the help of photos).
At home, the patient repeated the exercises with the help of the family and a mirror.
It was evaluated with the FGS at three months with photos and videos. He had accumulated a score of 54/100. At rest it showed the angle of the mouth stretched downwards, the Bell phenomenon absent. He closed his eye completely. During the voluntary movement, the lady was able to make simple movements and some wrinkles were not yet complete. He had difficulty showing his teeth (lower lip), holding the air in his mouth, kissing, blowing, pronouncing P, M, B, ("I eat baby food"). He still had mild sensitivity disorders in the lateral portion of the injured half-face.
In a third phase, to the exercises described so far, performed with greater autonomy and reducing the help of the therapist more and more, those with expressive purposes of III degree were added. Two short stories were chosen, and the patient learned to read them being careful to imitate the expressions indicated. At home, the patient repeated exercises such as holding air and moving with her mouth, repeating expressions in front of the mirror, uncovering her teeth, closing and opening her eyes, corrugating her forehead and eyebrows, reading and interpreting the dialogue in front of the mirror.
Results
After about 4 months from the beginning of the rehabilitation treatment, it was examined with the use of the FGS evaluation scale, totaling a score of 67 out of 100. There were no synkinesias, the recovery regarding the upper part of the face was faster than the mouth. The patient still showed insufficient movements of the lower part of the face. A slight sensitivity deficit persisted on the lateral surface of the injured half-life.
The last evaluation was carried out after just over 5 months. On the FGS scale, the patient scored 92/100. Symmetrical wrinkles were present around the mouth and nose, under the eyes and on the forehead. The lady was able to pout and smile when baring her teeth, albeit with a slight asymmetry in her lower lip. He closed and opened his eyelids with almost the same intensity. He was able to hold the food and move it inside his mouth.
The difficulty in blowing and kissing persisted even if in the slightest. The language had improved, in fact, he was able to pronounce: "Mangio pappe con mamma e papà" without any difficulty. There was no sensitivity deficit. He started to put on makeup and put on lipstick. She was calm, serene, not afraid of meeting people. He went back to work. He perceived his face light, soft while at the beginning he reported a sense of heaviness.
At a follow-up performed on resumption of work, after about 7-8 months after the intervention, a mild eye-mouth synkinesia appeared, which the patient was able to partially control, for which she resumed treatment.
Discussion
In the contemporary world, much attention is paid to the aesthetic-functional aspect and in particular to the condition of the face, a business card with which the individual presents himself in social interactions and in the workplace. The recovery of the motor activity of the affected half-face after facial injury is actually a complex process that cannot be considered only from a biomechanical perspective, but must contemplate multiple related aspects, such as non-verbal communication (mimic), the cognitive function- exploratory of some areas of the face, the function associated with chewing and swallowing.
The neurocognitive approach takes into account all these aspects and the latest discoveries such as the one concerning mirror neurons since we have seen how to observe an action, induces in those who observe the automatic simulation of movement. Indeed, for this type of approach, the use of the motor image is fundamental because thanks to it the subject senses the production of the gesture at a sensorial level, that is, he feels its tactile, kinaesthetic and pressure sensations, even without performing the movement.
It is conceivable that it is possible to limit an abnormal reinnervation during the nerve restart process if all the principles of this approach are respected, not requiring a voluntary activity from the patient unless the premises have been built beforehand through perceptual exercises only. In this way it is probably possible to progressively improve the quality of movement, the final goal of our treatment, avoiding pathological sequelae such as synkinesias and spasms.
Article Info
Article Type
Case ReportPublication history
Received: Mon 27, Apr 2020Accepted: Mon 11, May 2020
Published: Fri 29, May 2020
Copyright
© 2023 Mariaconsiglia Calabrese. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GCCR.2020.01.02
Author Info
M. Ciriello Mariaconsiglia Calabrese
Corresponding Author
Mariaconsiglia CalabresePhysiotherapy Degree Course, Department of Medicine, Surgery and Dentistry, University of Salerno, Società Italiana Fisioterapia e Riabilitazione, Baronissi, Italy
Figures & Tables




References
- Lotter M, Quinci A (2012) La riabilitazione delle paralisi periferiche del VII nervo cranico. Teorie e proposte terapeutiche. Padova: Piccin.
- Pavese C, Tinelli C, Furini F, Abbamonte M, Giromini E et al. (2013) Validation of the Italian version of the Sunnybrook Facial Grading System. Neurol Sci 34: 457-463. [Crossref]
- Atolini Junior N, Jarjura J, Junior J, De V, Gignon F et al. (2009) Facial Nerve Palsy: Incidence of Different Ethiologies in a Tertiary Ambulatory. Arch Otorhinolaryngol Intl Arch Otorhinolaryngol 1313: 175-167.
- Fargher KA, Coulson SE (2017) Effectiveness of electrical stimulation for rehabilitation of facial nerve paralysis. Phys Ther Rev 22: 169-176.
- Monini S, Iacolucci CM, Di Traglia M, Lazzarino AI, Barbara M (2016) Ruolo della riabilitazione Kabat nella paralisi del nervo facciale: Studio randomizzato su casi severi di paralisi di Bell. Acta Otorhinolaryngol Ital 36: 282-288.
- Peitersen E (2002) Bell’s palsy: The spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl 549: 4-30. [Crossref]
- Ryzenman JM, Pensak ML, Tew JM Jr (2005) Facial paralysis and surgical rehabilitation: A quality of life analysis in a cohort of 1,595 patients after acoustic neuroma surgery. Otol Neurotol 26: 516-521. [Crossref]
- Ahmed A (2005) When is facial paralysis Bell palsy? Current diagnosis and treatment. Cleve Clin J Med 72: 398-401, 405. [Crossref]
- Monini S, Buffoni A, Romeo M, Di Traglia M, Filippi C et al. (2017) Kabat rehabilitation for Bell’s palsy in the elderly. Acta Otolaryngol 137: 646-650. [Crossref]
- Baricich A, Cabrio C, Paggio R, Cisari C, Aluffi P (2012) Peripheral facial nerve palsy: how effective is rehabilitation? Otol Neurotol 33: 1118-1126. [Crossref]
- Pereira LM, Obara K, Dias JM, Menacho MO, Lavado EL et al. (2011) Facial exercise therapy for facial palsy: systematic review and meta-analysis. Clin Rehabil 25: 649-658. [Crossref]
- Ikeda M, Abiko Y, Kukimoto N, Omori H, Nakazato H et al. (2005) Clinical factors that influence the prognosis of facial nerve paralysis and the magnitudes of influence. Laryngoscope 115: 855-860. [Crossref]
- Kasahara T, Ikeda S, Sugimoto A, Sugawara S, Koyama Y et al. (2017) Efficacy of Tape Feedback Therapy on Synkinesis Following Severe Peripheral Facial Nerve Palsy. Tokai J Exp Clin Med 42: 139-142. [Crossref]
- Nicastri M, Mancini P, De Seta D, Bertoli G, Prosperini L et al. (2013) Efficacy of early physical therapy in severe Bell’s palsy: a randomized controlled trial. Neurorehabil Neural Repair 27: 542-551. [Crossref]
- Lotter M, Quinci A (1990) Proposta di condotta terapeutica per la riabilitazione delle paralisi del faciale. Riabilitazione e Apprendimento. Padova: Liviana Medicina.
- Miehlke A, Stennert E, Chilla R (1979) Processes of regeneration. Clin Plast Surg 465-470.
- Coulson SE, Croxson GR, Adams RD, O’Dwyer NJ (2005) Reliability of the “Sydney,” “Sunnybrook,” and “House Brackmann” facial grading systems to assess voluntary movement and synkinesis after facial nerve paralysis. Otolaryngol Head Neck Surg 132: 543-549. [Crossref]
- Ross BG, Fradet G, Nedzelski JM (1996) Development of a sensitive clinical facial grading system. Otolaryngol Head Neck Surg 114: 380-386. [Crossref]
- Fattah AY, Gurusinghe AD, Gavilan J, Hadlock TA, Marcus JR et al. (2015) Facial nerve grading instruments: Systematic review of the literature and suggestion for uniformity. Plast Reconstr Surg 135: 569-579. [Crossref]
- Gothard KM (2014) The amygdalo-motor pathways and the control of facial expressions. Front Neurosci 8: 43. [Crossref]
- Pagani R (2014) Emotional training of facial muscles after facial nerve palsy: a preliminary report Title. Neurol Sci Off J Ital Neurol Soc Springer 9.
- Brown MC, Holland RL, Ironton R (1980) Nodal and terminal sprouting from motor nerves in fast and slow muscles of the mouse. J Physiol 306: 493-510. [Crossref]
- Hennig R (1987) Late reinnervation of the rat soleus muscle is differentially suppressed by chronic stimulation and by ectopic innervation. Acta Physiol Scand 130: 153-160. [Crossref]
- Teixeira LJ, Valbuza JS, Prado GF (2011) Physical therapy for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev CD006283. [Crossref]
- Diels HJ (2000) Facial paralysis: is there a role for a therapist? Facial Plast Surg 16: 361-364. [Crossref]
- Rijntjes M, Tegenthoff M, Liepert J, Leonhardt G, Kotterba S et al. (1997) Cortical reorganization in patients with facial palsy. Ann Neurol 41: 621-630. [Crossref]
- Paolucci T, Cardarola A, Colonnelli P, Ferracuti G, Gonnella R et al. (2019) Give me a kiss! An integrative rehabilitative training program with motor imagery and mirror therapy for recovery of facial palsy. Eur J Phys Rehabil Med 56: 58-67. [Crossref]
- Gervasoni F, Pagani R, Cupello S, Cerri G, Previtera AM (2018) L’ emotional training nelle paralisi periferiche del nervo facciale. Minerva Riabilitativa.
- Baron MR (1977) L’esercizio terapeutico conoscitivo nella paralisi del VII nervo cranico. Riabilitazione e apprendimento. Napoli: Liviana Medicina.
- Baron MR (1977) Utilizzo dell’immagine nelle lesioni del VII nervo cranico. Riabilitazione e apprendimento. Napoli: Liviana Medicina.
- Lorigiola C, Quinci A (2001) Tempi e modalità dell’esercizio terapeutico nella rieducazione delle paralisi del VII nervo cranico. Riabilitazione cognitiva. Fornacette (Pi): Ars.
- Bateson G (2000) Verso un’ecologia della mente. Milano: Adelphi.
- Ekman P (2003) Emotions Revealed: Recognizing Faces and Feelings to Improve Communication and Emotional Life. New York: Times Book.
