Journals
The Value of Imaging Diagnostics in the Kimura’s Disease
A B S T R A C T
Kimura's disease (KD) is a benign chronic inflammatory disease of subcutaneous tissue of unknown etiology. Although it is regularly reported and is now clearly defined, it still constitutes a diagnostic challenge, as its resemblance with benign and malignant diseases can make the diagnosis difficult, requiring the skills of experienced pathologists. We report here our experience with Kimura's Disease, presenting two cases of female patients from Saudi Arabia with the pathology located within the orbit who were successfully treated surgically at Clarós Clinic. Afterwards we review the literature on the subject and discuss diagnostic process with particular emphasis on imaging diagnostic and treatment options to improve our understanding of this mysterious disease.
Keywords
Kimura's disease,orbital tumor,radiological imaging,angiolymphoid hyperplasia with eosinophilia,eosinophilic angiocentric fibrosis
Introduction
Kimura's disease (KD) is a rare benign inflammatory disease of subcutaneous tissue with a predilection to the head and neck region [1]. It occurs mainly in young and middle-aged Asian patients with 3,5:1 male to female ratio, however, a number of cases have also been reported among non-Asians [2, 3]. Although this condition is regularly described in the literature and is now clearly defined, it still remains a diagnostic challenge. A rare occurrence, as well as, resemblance with benign and malignant diseases make the diagnostic process insidious. Cooperation between clinician and an experienced radiologist and pathologist is not to be overestimated.
Materials and Methods
We present two similar clinical cases of a Kimura's disease located in the orbit. Both female patients received surgical treatment in Clarós Clinic between 2014 and 2019 with satisfying results. During the diagnosis contrast-enhanced computed tomography revealed extraconal orbital mass involving lacrimal gland. The extent of the disease differed in two cases however the histopathological examination showed the same features of Kimura's disease. Patients require continuous follow up due to the risk of recurrence. Afterward, we review the literature on the subject.
Case report 1
Previously we described a case of a 32-year-old Saudi Arabian woman who presented with a history of left upper eyelid swelling lasting 7 years before the underlying cause of her complaints was identified [4]. The initial diagnosis was a "fat cyst", which was operated under local anesthesia via a subpalpebral incision. Within three months symptoms recurred and biopsy was taken, however, the specimen was insufficient for histological examination. At that point, contrast-enhanced computed tomography was performed showing a mass located within the left orbit involving the lacrimal gland. Excision biopsy was taken via the upper eyelid. Description suggested differential diagnosis between eosinophilic angiocentric fibrosis (EAF) and granulomatosis with polyangiitis (GPA). The patient received a course of oral corticosteroids, which later had to be discontinued due to high blood pressure. Clinical presentation, slow but continuous progression of symptoms despite treatment and previous investigation weren"t conclusive of diagnosis, therefore, another biopsy was performed. The examination revealed angiolymphoid hyperplasia with eosinophilia characteristic of Kimura's disease. The patient was qualified for surgical treatment.
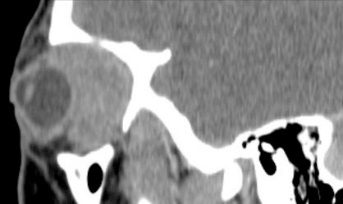
At that point, the patient contacted our clinic to get a second opinion. Within time symptoms progressed. Apart from the swelling of the left eyelid, she suffered from pain in the left eye on upward movement and irritation of conjunctiva. During the first appointment, visual acuity was 10/10 in the right eye (RE) and 8/10 in the left eye (LE). Intraocular pressure was within reference ranges (12 mmHg in the RE and 17 mmHg in the LE). Hertel examination revealed 5 mm difference between eyes (19 mm RE and 24 mm LE). LE was dislocated inferiorly, elevation was impaired, otherwise, eye motility was normal. The patient presented ptosis on the affected side. There was a visible scar from the previous operation on the upper eyelid. Palpation of the cervical area showed no signs of the salivary glands and lymph nodes pathology. We performed contrast-enhanced CT which showed an oval-shaped extraconal mass measuring 36 * 16 *24 mm with homogenous contrast enhancement and well-defined margins with no bone erosion (Figure 1 A, B and C). The tumor was located between the eyeball and the lateral wall of the orbit and there was lateral rectus muscle involvement. The laboratory analysis including complete blood count, eosinophilia, total IgE was within reference ranges. No risk factors were recorded in medical history and the general condition was good.
Figure 1: CT scan of the orbits. A: Axial section: demonstration of proptosis and inclusion of the lateral rectus muscle in the tumor. B: Frontal section: mass occupying the lateral quadrants of the orbit. C: Sagittal section: tumor location beyond the eyeball
Based on clinical data and imaging diagnostics, the patient was qualified for surgical treatment. The scope of the operation included a complete tumor excision by lateral orbitotomy via the modified Stallard-Wright incision within lid crease. Exposure of the lateral wall of the orbit was followed by the temporalis muscle elevation and the periorbital tissues dissection. In the next step, we performed osteotomy using a circular saw and a chisel. The bony fragment was preserved for further reconstruction. Exploration of the orbit revealed a firm, light, encapsulated mass in the area of the lacrimal gland expanding towards the lateral rectus muscle which was dissected and freed from its synechiae. We managed to resect the tumor in one piece.
In the postoperative period, we ordered 2 g of amoxicillin and clavulanic acid per day for one week combined with a 10-day course of methylprednisolone at a 1 mg/kg/day dose.
Proptosis and conjunctival erythema reduced. The abduction of the left eye remained deficient with persistent ptosis which required surgical correction at the later stage. Visual acuity remained stable. CT imagining performed 12 weeks after the surgery showed residual edema of the lateral rectus muscle (Figure 2). We examined the orbit with MRI 6 months later to exclude recurrence (Figure 3).
Figure 2: CT imagining performed 12weeks after the surgery showed residual edema of the lateral rectus muscle
Figure 3: MRI performed 6 months after the CT showed no sign of recurrence.
The microscopic picture confirmed Kimura's disease (follicular hyperplasia with numerous capillaries and arterioles surrounded by an intense fibrotic reaction arranged in concentric rings; lymphoid infiltration of interfollicular and perivascular zones, a small number of eosinophil leukocytes, associated with marked fibrosis within the lesion, absence of protrusion into the vascular lumen (Fig. 4) [4]).
Figure 4: Histological sections: Follicular hyperplasia with numerous capillaries and arterioles surrounded by an intense fibrotic reaction arranged in concentric rings; lymphoid infiltration of interfollicular and perivascular zones, a small number of eosinophil leukocytes, associated with marked fibrosis within the lesion, absence of protrusion into the vascular lumen.
At three-year follow-up, the patient was in good general condition. She underwent blepharoplasty to correct remaining ptosis in the affected eye. Long-term ophthalmological and otorhinolaryngological surveillance will be required supplemented by CT and MRI imagining due to the risk of recurrence.
Case report 2
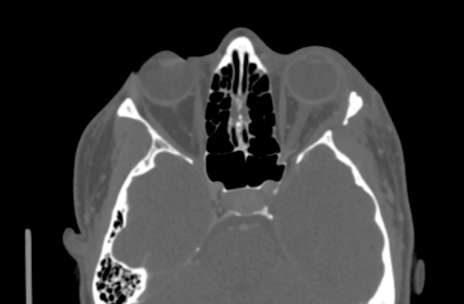
A 37-year-old woman referred to our clinic from Dubai presented with a 4-year history of proptosis and motility impairment in the left eye accompanied by palpebral edema. CT revealed a left extraconal orbital tumor measuring 46 x 29 x 31 mm with homogenous contrast enhancement involving the lacrimal gland, expanding towards and involving upper eyelid and all eye muscles except the middle and inferior rectus muscles and invading sclera. The optic nerve was displaced inferomedially (Figure 5 A,B,C). The patient complained of blurred vision, diplopia and ocular pain on the left side. At the initial examination visual acuity was 10/10 on the right side and 6/10 on the left. Intraocular pressure was slightly increased in the affected eye (23 mmHg). Hertel measurements showed 20mm in the RE and 29 mm in the LE. Restriction of eye movements in all directions was prominent and the eye was displaced inferolaterally. Examination of the salivary glands and lymph nodes was normal. Otherwise, the patient's general condition was good. The laboratory findings showed anemia. Eosinophilia and IgE level were normal.
Figure 5: CT scan of the orbits. A: Axial section: demonstration of exophthalmos and displacement of the eyeball. B: Frontal section: mass involving eye muscles. C: Sagittal section: tumor involving the lacrimal gland, expanding towards and involving upper eyelid.
Considering all above we performed biopsy through the eyelid which confirmed Kimura's disease, just like in the first case. The patient was further qualified for surgical treatment.
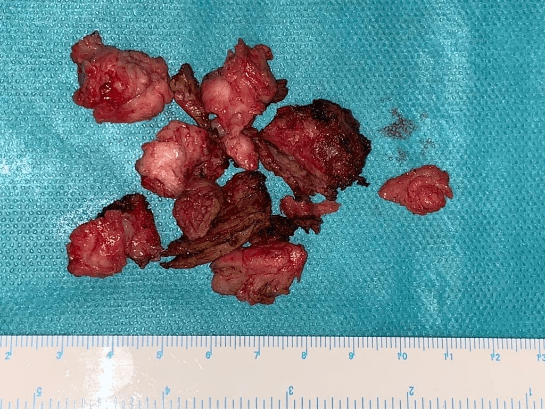
Lateral orbitotomy was performed under general anesthesia via a semicircular incision. The lateral wall of the orbit was exposed by elevating the temporalis muscle in the temporal fossa laterally and detaching the periorbital tissues. The osteotomy was performed with a circular saw. The periorbital tissues were incised showing a firm, whitish, tumor involving the lacrimal gland adherent to the lateral rectus, superior rectus, superior oblique, and inferior oblique muscles. The tumor was dissected and, after the muscles were released, removed together with part a of the lacrimal gland. In the next stage, an incision was made in the medial part of the upper eyelid and the second part of the tumor located in the palpebrae and medial aspect of the orbit was resected (Figure 6). Afterward, the wound was closed in 4 planes and a compressive dressing was applied. The patient was put on ciprofloxacin 2x500mg per day for 10 days and methylprednisolone at a dose of 1 mg/kg/day for 10 days.
Figure 6: A firm, whitish tumor removed during surgery.
The reduction of exophthalmos was noticed one day after the surgery as well as reduction of eyeball dislocation. After one-week double vision didn't improve, visual acuity and ocular motility remain impaired; however, more time is required to judge the final results. Histological examination confirmed the findings of the previous biopsy. The patient will be followed by ENT specialist and ophthalmologists. First post-op CT is planned 3 months after the operation.
Discussion
Kimura's disease is a benign inflammatory disease of subcutaneous tissue with the predilection to the head and neck region. First descriptions date back to 1937 China when Kim and Szeto identified a group of patients with this entity using the name of eosinophilic hyperplastic lymphogranuloma [1, 5]. Kimura provided a more detailed description in 1948 [6]. It is most common in young and middle-aged Asian man [2]. The origin remains unknown, however immunological disturbances involving abnormal T-cell stimulation has been described [1]. Subcutaneous nodules frequently associated with salivary gland and regional lymph node involvement are the typical manifestation of Kimura's disease. Location in the submandibular, retroauricular, mastoid, and cervical regions have also been reported as well as sporadic cases in the groin, orbit, axilla, and arm [2, 7].
Clinical features might overlap with those of broad spectrum of benign and aggressive entities such as Hodgkin's lymphoma, angioimmunoblastic T cell lymphoma, Langerhans cell histiocytosis, florid follicular hyperplasia, Castleman's disease, eosinophilic angiocentric fibrosis (EAF), granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA), drug-induced and parasitic lymphadenitis and angiolymphoid hyperplasia with eosinophilia (ALHE) [2, 7, 4].
Especially the last one caused a lot of confusion which results from their histological similarities [2]. However, clinical manifestation and epidemiology help to differentiate the entities. Kimura's disease affects young and middle-aged male Asians, presenting eosinophilia and high IgE level on laboratory tests. Clinical manifestation includes deep subcutaneous nodules and swelling with unchanged skin above the lesion associated with the involvement of the main salivary glands and lymph nodes [1-3]. ALHE, on the other hand, affects all ethnic groups with no sex predominance and a mean age of incidence about 38 years [8]. A predilection for the periauricular area and scalp is also characteristic [9]. Other common areas of involvement include oral mucous membranes, pharynx, and orbit. Patients present superficial erythematous or hyperpigmented dome-shaped dermal papules or pruritic or painful nodules of 2 to 3 cm diameter accompanied by bleeding. Lesions do not resolve spontaneously [9]. Regional lymphadenopathy, serum eosinophilia, and elevated IgE levels are uncommon in ALHE [1].
The microscopic distinction might be problematic as those two entities resemble each other. Contrary to Kimura's disease, in ALHE lymphoid infiltration is mild to moderate, the presence of lymphoid follicles is inconsistent. There is no folliculolysis, eosinophilic abscess formation, nor, common in Kimura's disease, fibrosis. Vascular proliferation is more marked with an arranged in a manner of "cobblestone" endothelial lining of plump, low cuboidal "epithelioid" or "histiocytoid" cells with acidophilic cytoplasm with vacuolization and vesicular nuclei. Vessels in Kimura's disease have thin walls with flat endothelial cells without "epithelioid" or "histiocytoid" cells [10]. The initial pathological report of our first patient indicated differential diagnosis between EAF and GPA.
Eosinophilic angiocentric fibrosis is a rare disease with slowly progressing symptoms. It usually presents as white to pink, fleshy submucosal mass or mucosal ulceration in the anterior nasal cavity. Sometimes it extends into the sinuses and causes bone destruction. In rare cases, the disease might be located in the larynx and lower respiratory tracts or orbit [11]. The origin is unclear, however, relation with allergy, previous trauma, and IgG4-related disease has been described. Histopathological characteristics include numerous eosinophils and, untypical for Kimura's disease "onion skin"fibrosis [12]. Additional tests might be used in diagnostically challenging cases. An increased number of IgG4+ plasma cells per high-power field and IgG4+:IgG ratio greater than 40% together with elevated IgG4 serum level is characteristical of IgG4-related disease. Complete surgical resection with or without systemic on local steroids remains the primary mode of treatment, however, Rituximab might be used in IgG4 related cases [11].
Granulomatosis with polyangiitis, previously Wegener granulomatosis, is a systemic condition affecting the upper and lower respiratory tract and kidneys in most cases, sometimes other organs as well. A small group of patients presents lesion in the head and neck only, without general symptoms (local GPA). The disease affects patients of all ages slightly more commonly men. Contrary to EAF and Kimura's disease clinical presentation is more aggressive with 5 months of mean survival time without treatment [13]. C-ANCA is specific for GPA on laboratory tests. Characteristic features on CT include bone destruction of the sinonasal region and mastoid cells, together with sclerosing osteitis and bone thickening. Microscopical examination shows granulomatous inflammation, scattered giant cells, vasculitis or necrotizing granulomata. Criteria of the American College of Rheumatology (ACR; 1990), are used to make the final diagnosis. Minimum 2 of following must be met: (1) sinus involvement; (2) lung X-ray showing nodules, a fixed pulmonary infiltrate or cavities; (3) urinary sediment with hematuria or red cell casts; and (4) histological granulomas within an artery or in the perivascular area of an artery or arteriole. Unlike KD and EAF immunosuppressive therapy is a standard treatment with surgery limited to non-responding cases of the localized disease. [13] .
The time between initial symptoms and the diagnosis in both presented patients lasted several years. The fact that they are both females without typical laboratory tests abnormalities was significant. The site of the disease was also untypical. In the first case, the initial surgical procedure without examination of removed tissue and the misleading pathological report of the second biopsy prolonged the diagnostic process. However, the first contrast-enhanced CT showed clearly demarcated orbital mass without bone invasion which should have favor complete surgical resection. A prolonged time of diagnosis may as well result from patient-related factors. Our second patient was ignoring her symptoms for almost a year before consulting a doctor and later on, she didn't follow his recommendations regarding detailed ophthalmological examination and imaging diagnostics. Our previous experience and comparison of CT and histological findings helped to make determine the disease.
In both patients computed tomography revealed extraconal tumor with homogenous enhancement on contrast and well-defined margins without bone invasion, involving lacrimal gland. Although findings are not specific, together with clinical presentation, might bring to mind the diagnosis of Kimura disease. Histological examinations were identical as well.
In both patients, the delay of Kimura's disease diagnosis led to a wider scope of surgical resection and left cosmetic and functional sequelae (ptosis), which required further treatment. Many authors agree that surgical resection is the treatment of choice for Kimura's disease [1-3]. In case of recurrence medical therapy, such as systemic steroids, and immunosuppressants have been tried [2, 14-16] Anti-IgE therapy-omalizumab has recently been used as a treatment in KD with promising effects [17]. Local, low-dose irradiation may also be applied, however, it's side effects along with benign nature of the disease limits its use as primary modality [18]. Despite its benign clinical and histopathological features, the recurrence rate is high in spite of treatment, therefore long-term follow-up is required [2, 3]. At our clinic, we performed contrast-enhanced CT supplemented by MRI.
Conclusion
Kimura's disease is a rare, benign, chronic inflammatory disease of the subcutaneous tissue with head and neck predilection. The origin remains unknown. Most commonly it presents as nodules located under the skin. Salivary gland and lymph node involvement are frequent. Diagnosis is very often based on the exclusion of the more common diseases. The orbit and the lacrimal gland involvement have been, so far, considered is a very rare location of this pathology. However, we managed to treat two female patients with such presentation within five years period. Despite the uncommon occurrence, this differential diagnosis shall be considered in any case of eosinophilic angiocentric fibrosis and angiolymphoid hyperplasia with eosinophilia especially in patients of Asian origin.
Disclosure of interest
The authors declare no conflict of interest.
Article Info
Article Type
Case ReportPublication history
Received: Tue 30, Apr 2019Accepted: Tue 16, Jul 2019
Published: Fri 26, Jul 2019
Copyright
© 2023 Clarós P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.RDI.2019.03.03
Author Info
Corresponding Author
Clarós PC. Los Vergós 31, 08017 Barcelona, Spain
Figures & Tables







References
- Abuel-Haija M, Hurford MT (2007) Kimura disease. Arch Pathol Lab Med 131: 650-651. [Crossref]
- Chen H, Thompson LD, Aguilera NS, Abbondanzo SL (2004) Kimura disease: a clinicopathologic study of 21 cases. Am J Surg Pathol 28: 505-513. [Crossref]
- Li TJ, Chen XM, Wang SZ, Fan MW, Semba I (1996) Kimura's disease: a clinicopathologic study of 54 Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82: 549-555. [Crossref]
- Clarós P, Fokouo V, Nyada F, Clarós A (2017) Kimura's disease of the orbit: A modern diagnostic challenge. Eur Ann Otorhinolaryngol Head Neck Dis 134: 287-289. [Crossref]
- Kim H., Szeto C (1937) Eosinophilic hyperplastic lymphogranuloma, comparison with Mikulicz's disease. Chinese Medical Journal 23: 699-700.
- Kimura T, Yoshimura S, Ishikawa E (1948) On the unusual granulation combined with hyperplastic changes of lymphatic tissue. Trans Soc Pathol Jpn 37: 179-180.
- Shetty AK, Beaty MW, McGuirt WF, Woods CR, Givner LB (2002) Kimura's disease: a diagnostic challenge. Pediatrics 110: e39. [Crossref]
- Adler BL, Krausz AE, Minuti A, Silverberg JI, Lev-Tov H (2016) Epidemiology and treatment of angiolymphoid hyperplasia with eosinophilia (ALHE): A systematic review. J Am Acad Dermatol 74: 505-512. [Crossref]
- Prathyusha Chitrapu, Mahir Patel, Allison Readinger, Alan Menter (2014) Angiolymphoid hyperplasia with eosinophilia. Proc (Bayl Univ Med Cent) 27: 336-337. [Crossref]
- Sah P, Kamath A, Aramanadka C, Radhakrishnan R (2013) Kimura's disease - An unusual presentation involving subcutaneous tissue, parotid gland and lymph node. J Oral Maxillofac Patholo 17: 455-459. [Crossref]
- Ahn J, Flanagan M, (2018) Eosinophilic Angiocentric Fibrosis: A Review and Update of Its Association with Immunoglobulin G4-Related Disease. Arch Pathol Lab Med 142: 1560-1563. [Crossref]
- Heft Neal ME, Rowan NR, Willson TJ, Wang EW, Lee SE (2017) A Case Report and Systematic Review of Eosinophilic Angiocentric Fibrosis of the Paranasal Sinuses. Ann Otol Rhinolo Laryngolog 126: 415-423 [Crossref].
- Joanna Wojciechowska, Wojciech Krajewski, Piotr Krajewski, Tomasz Kręcicki (2016) Granulomatosis with Polyangiitis in Otolaryngologist Practice: A Review of Current Knowledge. Clin Exp Otorhinolaryngol 9: 8-13. [Crossref]
- Armstrong WB, Allison G, Pena F, Kim JK (1998) Kimura's disease: two case reports and a literature review. Ann Otol Rhinol Laryngol 107: 1066-1071. [Crossref]
- Kaneko K, Aoki M, Hattori S, Sato M, Kawana S (1999) Successful treatment of Kimura's disease with cyclosporine. J Am Acade Dermatol 41: 893-894. [Crossref]
- Archana MV, Shenoy KV, Cherian EV, Shetty K (2014) Steroid therapy in Kimura's disease. Muller J Med Sciences Research. 5: 77-79.
- Nonaka M, Sakitani E, Yoshihara T (2014) Anti-IgE therapy to Kimura’s disease: a pilot study. Auris Nasus Larynx 41: 384-388. [Crossref].
- Hareyama M, Oouchi A, Nagakura H, Asakura K, Saito A et al. (1998) Radiotherapy for Kimura's disease: the optimum dosage. Int J Radiat Oncol Biol Phys 40: 647-651. [Crossref]
