Thrombolytic Treatment in High-Risk Pregnancy: A Case Report
A B S T R A C T
Ischemic stroke during pregnancy occurs most often in the third trimester and is potentiated by an increased pro-coagulant state during pregnancy. Precisely this procoagulant state, associated with other thrombophilic phenomena and various risk factors for cardio- and cerebro-vascular pathologies, is the basis of a stroke in the elderly pregnant woman. A 43-year-old woman of 30 weeks pregnant presented within 120 minutes of the sudden onset of left side hemiparesis was given thrombolytic treatment with recombinant tissue plasminogen activator. The risk was extremely high since in the past she had a premature birth for unknown reasons. Our patient improved clinically with no residual deficits. But, being at risk, she was transferred to another hospital where she spontaneously gave birth, after a few days, to a healthy premature baby. It is reasonable to weigh in the benefit of alteplase vs. the risk in this patient group and give treatment for disabling stroke, particularly if there is no access to endovascular treatment.
Keywords
Stroke, pregnancy, thrombolysis, elderly
Background and Aims
Even though the incidence of stroke in pregnancy and the puerperium appears to be increasing, ischemic stroke is relatively uncommon in fertile women. Probably due to women delaying pregnancy until older ages as well as increasing rates of risk factors as obesity, diabetes and hypertension, we are observing that pregnancies can be hindered along their course [1, 2]. Ischemic stroke during pregnancy occurs most often in the third trimester and is potentiated by an increased pro-coagulant state during pregnancy [3]. Precisely this procoagulant state, associated with other thrombophilic phenomena and various risk factors for cardio- and cerebro-vascular pathologies, is the basis of a stroke in the elderly pregnant woman. Guidelines indicate thrombolysis as one of the treatments for stroke during pregnancy. Actually, treatment is often delayed or not given, because of highlighted relative contraindications. The major risks are maternal hemorrhagic complications [1, 4-9].
Case Report
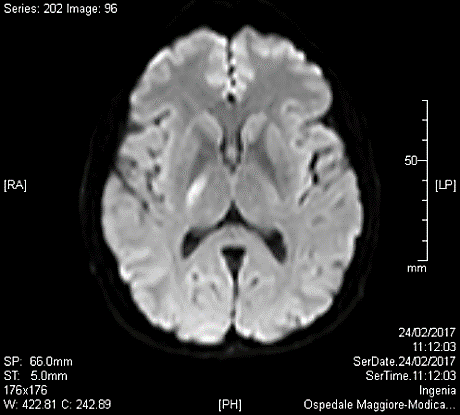
In the emergency room of the hospital where I used to work, Vittoria (Ragusa), a 43-year-old woman, 30 weeks pregnant, presented within 120 minutes of abrupt onset of left-sided hemiparesis. Not being able to undergo CT scan for pregnancy, diffusion-weighted imaging MRI showed an ischemic area at the posterior arm of the right internal capsule (Figure 1) and given that her clinical conditions were getting worse, it was decided, with obstetric back-up and according to recent indications, to treat her with IV rTPA (recombinant tissue plasminogen activator), in the absence of availability of the interventional neuroradiology unit in the area of the hospital. Electrocardiogram and vital signs were normal. Blood tests showed leukocytosis (11,900 mm3) and fibrinogen (485 mg/dL), total cholesterol 272 mg/dl, triglycerides 299 mg/dl, anti-nucleus antibodies (ANA) 1:160, free protein S 37%. The other blood tests were within normal limits. During and after thrombolytic treatment, the patient was monitored and kept under close clinical observation.
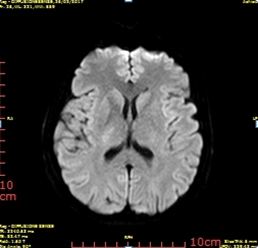
The response was excellent and at the end of thrombolysis she was able to move the left side of her body. Our patient improved clinically with no residual deficits and there was no evidence of fetal injury following administration of rtPA on follow-up obstetrical evaluations. In the following hours, shortly before her transfer, the patient began to complain of severe headache, nausea and a sensation of heat spread throughout the body. After performing a second MRI (Figure 2) and not having observed any clinical deterioration, it was decided to continue the clinical observation and to use an antiemetic drug with resolution of the symptoms. Due to a previous premature delivery (28 weeks), she was at risk of bleeding and death. Therefore, after treatment, she was transported to another hospital equipped with a neonatal intensive care unit. After 5 days, with a preterm delivery with a good outcome, she gave birth to a healthy baby.
Figures 1: MRI performed at a distance of three hours of symptom onset showed a restriction area of proton diffusivity in diffusion-weighted imaging (DWI), having lenticular morphology of about 15 mm, with consensual reduction of the values of the apparent diffusion coefficient. The angiographic sequences showed no significant alterations in caliber and course of the main vessels of Willis.
Figures 2: MRI performed 24 hours after the acute event: small area of altered signal at the posterior arm of the right internal capsule.
Discussion and Conclusion
It is well known as necessary and important physiologic changes are responsible for an increased risk of thrombotic complications during and after the pregnancy. They occur in hemostasis to prevent remarkable hemorrhage during delivery and allow for an increase and maintain the maternal–fetal circulations. The hypercoagulable state of pregnancy is common during pregnancy and augments the risk of certain complications due to an increase of pro-clotting factors, a reduction in natural thrombolytic activity and a lowering in anticoagulant protein activity (activated protein C, protein S). A normal hemostatic pattern usually returns 3-4 weeks following delivery. Given that there are no specific trials and the literature to guide our decision making is limited, since the angiographic team is not on site, this case confirms once again that acute stroke treatment decision-making is a complex process that must be performed quickly, particularly when certain conditions require rapidity of action and thought [9, 10].
In this case, if the patient must be treated at a first level stroke center, transport to an advanced stroke center as a “drip and ship” has to become a standard. It is important to emphasize that in pregnant women treated for ischemic stroke or other embolic conditions, complication rates of rtPA are found to be similar when compared to non-pregnant women (7-9% mortality). It is reasonable to weigh in the benefit of alteplase vs. the risk in this patient group and give treatment for disabling stroke, particularly if there is no access to endovascular treatment. In the near future, with the current ongoing implementation of mechanical thrombectomy in routine practice, it is expected that more pregnant women will benefit from acute reperfusion strategies.
Article Info
Article Type
Case ReportPublication history
Received: Tue 14, Apr 2020Accepted: Tue 12, May 2020
Published: Fri 15, May 2020
Copyright
© 2023 Enzo Sanzaro. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2020.02.06
Author Info
Corresponding Author
Enzo SanzaroDepartment of Neurology and Stroke Unit of Umberto I Hospital, Siracusa, Italy
Figures & Tables
References
- Cauldwell M, Rudd A, Nelson Piercy C (2018) Management of stroke and pregnancy. Eur Stroke J 3: 227-236. [Crossref]
- Kaur L, Puri M, Kaushik S, Sachdeva MP, Trivedi SS et al. (2013) Genetic thrombophilia in pregnancy: a case-control study among North Indian women. J Thromb Thrombolysis 35: 250-256. [Crossref]
- Mantoan Ritter L, Schüler A, Gangopadhyay R, Mordecai L, Arowele O et al. (2014) Successful thrombolysis of stroke with intravenous alteplase in the third trimester of pregnancy. J Neurol 261: 632-634. [Crossref]
- Gartman EJ (2013) The use of thrombolytic therapy in pregnancy. Obstet Med 6: 105-111. [Crossref]
- Broderick JP (2013) Should intravenous thrombolysis be considered the first option in pregnant women? Stroke 44: 866-867. [Crossref]
- Li Y, Margraf J, Kluck B, Jenny D, Castaldo J (2012) Thrombolytic therapy for ischemic stroke secondary to paradoxical embolism in pregnancy: a case report and literature review. Neurologist 18: 44-48. [Crossref]
- Steinberg A, Moreira TP (2016) Neuroendocrinal, Neurodevelopmental, and Embryotoxic Effects of Recombinant Tissue Plasminogen Activator Treatment for Pregnant Women with Acute Ischemic Stroke. Front Neurosci 10: 51. [Crossref]
- Tassi R, Acampa M, Marotta G, Cioni S, Guideri F et al. (2013) Systemic thrombolysis for stroke in pregnancy. Am J Emerg Med 31: 448.e1-448.e3. [Crossref]
- Tversky S, Libman RB, Reppucci ML, Tufano AM, Katz JM (2016) Thrombolysis for Ischemic Stroke during Pregnancy: A Case Report and Review of the Literature. J Stroke Cerebrovasc Dis 25: e167-e170. [Crossref]
- Ritchie J, Lokman M, Panikkar J (2015) Thrombolysis for stroke in pregnancy at 39 weeks gestation with a subsequent normal delivery. BMJ Case Rep 2015: bcr2015209563. [Crossref]
