Tooth Loss Evolution in a Cohort Study of Type 2 Diabetic Patients (2012 -2016) Shows a Steady High Rate of Tooth Extractions Despite Oral Prevention Measures
A B S T R A C T
Aims: To assess tooth loss evolution in a population of type 2 diabetic patients over a 4-year follow up period in regard to their dental and medical follow ups.
Methods: Using a national data base of a French population of railways transport workers, we conducted a cohort analysis on the same population of diabetic patients by comparing 2016 data to previously analyzed 2012 results. Evolution of oral health was provided by descriptive analysis of tooth extractions and the frequency of scaling-prophylaxis through descriptive analysis, regarding medical and dental appointments evolution over the time lapse.
Results: Tooth extraction rates remain high for the diabetic patients in 2016 compared to the control population. Tooth loss occurs on average in a ten-year older age-range population, than in 2012. Dental appointments and scaling prophylaxis sessions frequencies significantly improved between 2012 and 2016.
Conclusion: Over a 4 year-follow up period of time, data analysis of type 2 diabetic patient population shows a steady and high rate of dental extractions. While scaling prophylaxis sessions and dental appointments contribute to delay tooth loss, they failed to treat or eradicate the dental condition of tooth loss in the diabetic patients.
Keywords
Type 2 diabetes, cohort study, oral health, tooth loss, periodontitis
Introduction
Diabetes is an increasingly prevalent chronic disease and a widely recognised factor for systemic complications [1]. Oral tissues resulting are affected by diabetes and periodontitis is recognized as the sixth complication of diabetes [2] and is a major cause of tooth loss in adults [3]. Periodontitis and diabetes are both chronic diseases with an established bidirectional relationship [4, 5]. However, such increased risk is controversial [6] and diabetes would not be direct etiologic factor but a predisposing factor for periodontal disease. Poorly controlled diabetic patients are three times more likely to develop chronic periodontitis compared to healthy subjects, despite similar subgingival biofilm [7, 8]. To some extend the control of periodontal inflammation can enhance the glycemic control; conversely active periodontal disease is more frequently seen in poorly controlled diabetic patients [9]. The effect of periodontitis on diabetes may be explained by the increase in levels of systemic pro inflammatory mediators, which exacerbates insulin resistance [10]. Evidence for treatment-benefits is disputed due to the variety of the sample population, evaluation of periodontal status and control of type 2 diabetes. Appropriate periodontal care can produce beneficial effects on metabolic outcomes among Diabetes Mellitus (DM) patients [11].
A meta-analysis of 9 randomised clinical trials found a moderate reduction in Haemoglobin A1c among DM patients after non-surgical periodontal treatment [12]. Another meta-analysis demonstrated that there was 0.29% reduction in Haemoglobin A1c with periodontal care at 3-4 months. It has been reported that non-surgical periodontal treatment improved systemic oxidative stress balance and quality of life but did not decrease HbA1c levels at 3 months follow-up [13]. Moreover, a meta-analysis of 9 clinical trials observed that periodontal treatment resulted in the reduction of inflammatory biomarkers such as tumour necrosis factor alpha and C-reactive protein in diabetic patients [14]. However, there is no evidence that this is sustained over the long term and reduces the prevalence of long-term complication such as tooth loss [15].
Tooth loss prevalence among middle-aged adults with chronic diseases reproduces a reality of poor oral health when compared with a systemically healthy population [16]. Several studies recently underlined the number of missing teeth as a possible predictive factor for cardiovascular events or death rate in diabetic patients [17]. Diabetes increases the risk of cardiovascular disease especially in patients with severe periodontitis [18]. This penchant was also observed in previous re¬searches that demonstrated a significantly higher preva-lence of tooth loss in individuals with diabetes [19, 20]. Previously and through data base analysis we had reported that tooth extractions occur at specific age range in type 2 diabetic patients [21]. Follow up of diabetic patients in regard to targeted organ complications are difficult to set up and few cohort studies have looked at oral health in these populations.
Here we report the database analysis of the same population of diabetic patients analyzed at a 4-year interval (2016 data versus 2012) compared to non-diabetic patients, who benefited from a common medical insurance coverage with equal access to preventive measures, in regard to periodontal diseases and medical care. We compared 2016 to 2012 oral health data estimated from tooth extractions and annual prophylaxis sessions and dental initial appointments. The aim of this study was to provide a follow up analysis of oral health and tooth loss pattern evolution and to address the effectiveness of preventive control measures in a population over a 4 year-timespan of type 2 diabetic patients.
Materials and Methods
The study involved analysis of the CPRP database (2016) for diabetic and non-diabetic patients. The data base and retrieval of the data were similar those previously described for the 2012 analysis. Briefly, the CPRP database is a national independent and specific database for French workers in the national railways network (SNCF) benefiting from a corporate medical insurance coverage.
According to the French health coverage system, a patient can be registered as a chronic- diseased patient, by his physician, for one of the registered medical conditions which involve continuous medical care throughout life. Following this registration, all the medical expenses related to the disease become fully covered by the insurance system. The patient is registered for a 5-year period and has to be re-entered at the end of this time lapse. Diabetic patients are registered according to the criteria for diabetes (ICD 10: E10-E14) in the WHO classification for chronic diseases, ICD (International Statistical Classification of Diseases and Related Health Problems). The patient can only be registered at the time when antidiabetic medications are initiated, and specific pharmacological expenses are needed. At the diet control stage of the disease, the patients are covered by the general French health coverage system and are not specifically registered. Therefore, the type 2 diabetic patients, considered in this study, comprise only those managed by oral hypoglycaemics, and those who were initially treated with oral hypoglycaemics and then go onto management with insulin.
The aim of the study was to study the 2016 outcome and compare it to the 2012 results; therefore, we considered the 2016 status of the 2012 diabetic population (D) that was a closed population. Newly registered diabetic patients between 2012 and 2016 were not included in the D population (closed cohort). Thus, the following populations 2012 and 2016 were considered in the database:
i. All CPRP population: (A) 2012 and 2016.
ii. Type 2 Diabetic population: (D) 2012 and 2016 closed cohort D.
iii. Non-diabetic free of chronic disease: (ND-FCD) 2012 and 2016.
Two populations were compared for the study of dental outcomes:
i. Population D, Type 2 diabetic patients only, 2012 and 2016 closed cohort.
ii. Population ND-FCD, all other subjects not registered as diabetic patients and without any other registered chronic disease.
As previously reported, populations were stratified by age and sex. We used the WHO standard age groups for the data retrieval. For purposes of comparison, the WHO Standard age group 80+ is an aggregate of the age groups 80-85, 85-89, 90; similarly, age group 0-9 is an aggregate of the age groups 0-4 and 5-9. The CPRP database also comprises all the coded medical and dental procedures for the affiliated members, since it provides for their medical expenses. Data managers sorted out the specific codes for the following dental outcomes: - teeth extractions (excluding 3rd molars) as an indicator of tooth loss, - scaling-prophylaxis sessions as an indicator of the initial periodontal therapy, which is included in the dental coverage of the French insurance system. Prevalence rates and relative risks compared the diabetic population (D) in regard to the non-diabetic population (ND-FCD). In addition, we further analyzed the data base for the dental appointments for the populations. We checked the annual number of initial dental appointments that comprise the initial checkup and diagnosis work out. Mortality rate and lost to follow up 2012 – 2016 were calculated in the diabetic population between 2012 and 2016.
All participants from population D 2016 (closed population 2012) and population ND-FCD (2016) were included in the analysis. Prevalence rates and relative risks compared the diabetic population (D) regarding the non-diabetic population (ND-FCD). Statistical analysis of the data was performed by the dental department of the CPRP-SNCF using the Pearson Chi Square (χ²) distribution comparison tests and, Student's (t) average comparisons. The 95% confidence intervals use the normal law and the binomial law for small numbers. The significance level is set at p = 0.05. Overall data were collected and analysed by the medical and dental department of the CPRP SNCF. The collection and processing of the data for this study were approved by the national French data protection authority (National Committee for Processed Data and Freedom-CNIL).
Table 1: Populations 2012-2016.
|
|
2012 |
2016 |
|||||||||
|
|
n |
% of sample |
mean age (yrs.) |
SD |
Confidence Intervals 95% confident |
|
n |
% of sample |
mean age (yrs.) |
SD |
Confidence Intervals 95% confident |
|
All (A) |
533 378 |
100 |
46.33 |
26.42 |
[46.26;46.40] |
All (A) |
499 943 |
100 |
46.43 |
26.50 |
[46.36 ; 46.51] |
|
Female |
179 671 |
33.69 |
42.11 |
29.34 |
[41.97;42.25] |
Female |
163 908 |
32.79 |
41.71 |
29.28 |
[41.57 ; 41.85] |
|
Male |
353 707 |
66.31 |
48.44 |
24.57 |
[48.36;48.52] |
Male |
336 035 |
67.21 |
48.74 |
24.70 |
[48.66 ; 48.82] |
|
Non diabetic - free chronic disease (ND-FCD) |
377 207 |
70.72a |
39.48 |
24.38 |
[39.40;39.56] |
Non diabetic - free chronic disease (ND-FCD) |
383363 |
76.69a |
38.9 |
24.07 |
[38.83;38.98] |
|
Female |
132 997 |
35.26 |
35.52 |
26.63 |
[35.38;35.66] |
Female |
132 029 |
34.44 |
35.71 |
26.15 |
[35.57;35.85] |
|
Male |
244 210 |
64.74 |
41.63 |
22.78 |
[41.54;41.72] |
Male |
251 334 |
65.56 |
41.35 |
22.9 |
[41.26;41.44] |
|
Type 2 Diabetic (D) |
27 305 |
5.12b |
71 |
11.2 |
[69.87;71.13] |
Type 2 Diabetic (closed cohort D) |
22 096 |
4.42b |
72.61 |
10.75 |
[72.46 ; 72.75] |
|
Female |
6562 |
24.03 |
74 |
12.2 |
[73.74;74.34] |
Female |
5180 |
23.44 |
75.41 |
12.04 |
[75.08;75.74] |
|
Male |
20743 |
75.97 |
70 |
10.6 |
[69.87;70.16] |
Male |
16916 |
76.56 |
72.15 |
10.2 |
[72.00;72.31] |
|
Type 2 Diabetic mortality rate 2012-2016 |
5 139 |
18.82c |
82.08 |
9.4 |
[81.83 ; 82.34] |
Type 2 Diabetic lost to follow up 2012-2016 |
70 |
0.26 |
|
|
|
|
Female |
1341 |
26.09 |
86 |
8.37 |
[85.63;86.52] |
Female |
41 |
0.62 |
|
|
|
|
Male |
3798 |
73.91 |
80.7 |
9.33 |
[80.38;80.97] |
Male |
29 |
0.14 |
|
|
|
a % of sample: ND-FCD population represents % of all CPR population.
b % of sample: Type 2 diabetic population represents % of all CPR population.
c % of sample: Type 2 diabetic mortality rate represents % of 2012 Type 2 diabetic population.
Results
The baseline characteristics of the population are shown in (Table 1). In 2016 the over whole CPRP population (A) comprises 499 943 individuals with a mean age at 46.43 years (SD: 26.50). As compared to the 2012 population, the population has decreased (-6.27%), mean age remained alike 2012; the sex ratio modified over time with and increased proportion of men over women (p<000.1) In 2016, the closed population of the 2012 type 2 diabetic population (D) (n=22 096) represents 4.42 % of population A with a mean age at 72.61 years (SD: 10.75); the non-diabetic – free of chronic disease population (ND-FCD) accounts for 76.69% of population A with a mean age at 38.9 years (SD: 24.07). The male-female percentages are 67.21%/32.79% in population A, 65.56%/34.44% in population ND-FCD and 76.56%/23.44% in the Type 2 diabetic population (D). The younger age and the over representation of males to females in the ND-FCD population reflects the insurance coverage of both active and retired railways workers and their direct family (spouse and children under 18).
Between 2012 and 2016, characteristics of the populations A and NDFCD were modified: the NDFCD population increased by 1.63%, with a younger age (38.9 years in 2016, versus 39.48 in 2012, p<0.001) and a slight titling sex ratio towards male (65.56% male / 34.44 % female in 2016, versus 64.74% / 35.26% in 2012, p<0.001). In 2016, the following changes are noted in the 2012 D population: while the sex ratio remains unchanged, the mean age has significantly increased (71 yrs. versus 72.6 yrs. p<0.001); 5139 individuals died in the time period, which is 18.82% of the sample with a mean age at 82.08 years (SD: 9.4). Mean age at death and mortality rate is higher for female than male patients (0.20 versus 0.18). Therefore, the annual death rate in the D population is at 0.047 for the diabetic patients. In addition, 70 individuals (0.26%) were lost to follow up, likely by changing their health coverage system.
2016 tooth extraction and scaling session’s results with the variations 2012-2016 are presented in (Table 2) for both the D population and the NDFCD. A statistically significant higher prevalence (p<0.01) is noted for D population’s tooth extractions in the 60 to 64 and above 70 age-ranges. Both in 2012 and 2016, the ND-FCD population, the extraction rate steadily increases with age. In 2016 the Type 2 diabetic population ratio for extraction remains as in 2012 twice that of the non-diabetic population (0.20 as opposed to 0.08, p < 0.01). Scaling prophylaxis sessions increase between 2012 and 2016 for diabetic patients (+26%, p<0.01). A significant increase (p < 0.01) is noted in the 45-49 age range and above 60 (60-79 range). In the NDFCD population there is an overall increase (+26%, p<0.01) in the annual number of scaling professional sessions at all ages, which may be related to the prevention campaigns initiated by the CPR in 2011 aimed at periodontal prevention in all patients.
Table 2: Ratio of teeth extractions and scaling-prophylaxis sessions among the two populations by age group in 2016 and change 2016/2012.
|
Populations 2016 |
Scaling prophylaxis sessions 2016 |
Tooth extractions 2016 |
||||||||||||||
|
DT2 |
ND-FCD |
DT2 |
ND-FCD |
|
DT2 |
NDFCD |
|
|||||||||
|
Age |
n |
n |
nb of scaling sessions |
ratio |
change 2016/ 2012 |
nb of scaling sessions |
ratio |
change 2016/ 2012 |
RR |
nb of tooth extractions |
ratio |
change 2016/ 2012 |
nb of tooth extractions |
ratio |
change 2016/ 2012 |
RR |
|
[0;9] |
0 |
54576 |
0 |
0 |
0 |
1901 |
0.03 |
-0.12** |
0.00 |
0 |
0 |
0 |
41 |
0.00 |
-0.97** |
0.00 |
|
[10;14] |
0 |
29242 |
0 |
0 |
0 |
4878 |
0.17 |
0.39** |
0.00 |
0 |
0 |
0 |
785 |
0.03 |
-0.74** |
0.00 |
|
[15;19] |
2 |
25293 |
0 |
0 |
-1 |
6164 |
0.24 |
0.27** |
0.00 |
2 |
1 |
0 |
329 |
0.01 |
-0.11 |
76.88 |
|
[20;24] |
10 |
24395 |
7 |
0.70 |
-0.13 |
7549 |
0.31 |
0.05** |
2.26 |
0 |
0 |
0 |
449 |
0 .02 |
-0 .19** |
0.00 |
|
[25;29] |
11 |
19628 |
1 |
0.09 |
-0.83* |
7156 |
0.36 |
0.12** |
0.25 |
0 |
0 |
-1 |
707 |
0.04 |
0.04 |
0.00 |
|
[30;34] |
14 |
19187 |
1 |
0.07 |
-0.61 |
7793 |
0.41 |
0.04* |
0.18 |
1 |
0.07 |
-0.04 |
872 |
0.05 |
-0.16** |
1.57 |
|
[35;39] |
36 |
22007 |
11 |
0.31 |
-0.36 |
10252 |
0.47 |
0.12** |
0.66 |
3 |
0.08 |
-0.11 |
1236 |
0.06 |
-0.09* |
1.48 |
|
[40;44] |
108 |
25420 |
50 |
0.46 |
-0.11 |
12252 |
0.48 |
0.26** |
0.96 |
12 |
0.11 |
-0.55 |
1727 |
0.07 |
-0.03 |
1.64 |
|
[45;49] |
147 |
17965 |
85 |
0.58 |
0.58** |
10178 |
0.57 |
0.31** |
1.02 |
15 |
0.10 |
-0.16 |
1671 |
0.09 |
-0.08* |
1.10 |
|
[50;54] |
401 |
20240 |
103 |
0.26 |
-0.23** |
8627 |
0.43 |
-0.02 |
0.60** |
65 |
0.16 |
0.13 |
2309 |
0.11 |
-0.12** |
1.42 |
|
[55;59] |
1511 |
33984 |
496 |
0.33 |
-0.01 |
17268 |
0.51 |
0.15** |
0.65** |
346 |
0.23 |
0.15 |
4814 |
0.14 |
-0 .07** |
1.62** |
|
[60;64] |
2704 |
28637 |
989 |
0.37 |
0.27** |
15853 |
0.55 |
0.48** |
0.66** |
579 |
0.21 |
0.20 |
4703 |
0.16 |
0.03 |
1.30** |
|
[65;69] |
3507 |
20077 |
1126 |
0.32 |
0.32** |
10229 |
0.51 |
0.54** |
0.63** |
636 |
0.18 |
-0.04 |
3564 |
0.18 |
0 .05 |
1.02 |
|
[70;74] |
3672 |
14803 |
1171 |
0.32 |
0.52** |
6859 |
0.46 |
0.49** |
0.69** |
770 |
0.21 |
0.15 |
2686 |
0.18 |
0 .00 |
1.16** |
|
[75;79] |
3590 |
10788 |
920 |
0.26 |
0.56** |
4331 |
0.40 |
0.57** |
0.64** |
808 |
0.23 |
0.27 |
2288 |
0.21 |
0 .06 |
1.06 |
|
80+ |
6383 |
17121 |
1112 |
0.17 |
0.51** |
4395 |
0.32 |
0.99** |
0.68** |
1134 |
0.18 |
0.11 |
3098 |
0.18 |
0.05 |
0.98 |
|
Total |
22096 |
383363 |
6072 |
0.27 |
0.26** |
135685 |
0.35 |
0.26** |
0.78** |
4371 |
0.20 |
0.13 |
31279 |
0.08 |
-0.13** |
2.42** |
NS : No statistical Significance *p<0,05 **p<0,01.
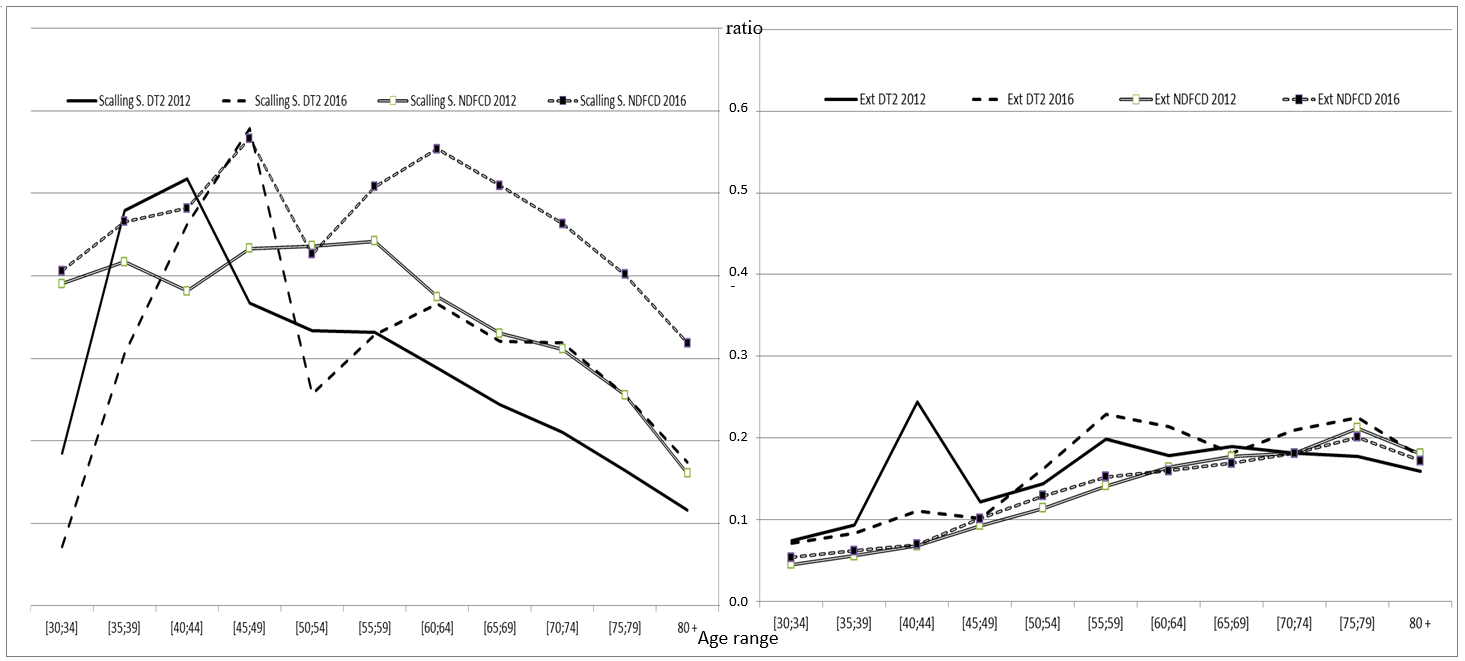
Figure 1: Comparative graphic curve of teeth extractions and scaling-prophylaxis sessions in 2012 and 2016 among the two populations by age group from 30 years to 80 years.
The overall trends for tooth extraction and scaling prophylaxis sessions are presented in (Figure 1). The extractions ranges with significant peak in increase have been delayed by about 10 years (40-44 in 2012, versus 55-59 and above in 2016). Between 2012 and 2016, in the DT2 population and as opposed to the NDFCD population, specifically it is noted that professionally active patients (20 to 44 age range) tend to have less scaling prophylaxis sessions than retired patients (above 60 yrs.). The results for outpatient dental appointments are presented in (Table 3). Medical appointments results could not be adequately compared between 2012 and 2016, since French guidelines in the care of diabetic patients have been modified in the interval, resulting in a different pattern of specialist referrals. In 2016 and similarly to 2012 on average, type 2 diabetic patients seek less advice than the ND-FCD population (annual ratio at 0.15 versus 0.16, p < 0.01), albeit a general increase in dental appointments is noted in 2016: for the NDFCD population in the range 0-19, and above 55, to a lesser extend at the following age ranges in the D population: 45-49 et 51-54, and 65-69 – 70-74, (p < 0.01).
Table 3: Outpatient dental appointments into the two populations in 2016.
|
|
DT2 dental consultations |
NDFCD dental consultations |
||||||
|
|
2016 |
|
|
2016 |
|
|
||
|
Age |
nb of dental consultations |
ratio |
change 2016/2012 |
nb of dental consultations |
ratio |
change 2016/2012 |
||
|
[0;9] |
0 |
0 |
0 |
|
8505 |
0.16 |
0.18 |
** |
|
[10;14] |
0 |
0 |
0 |
|
6730 |
0.23 |
0.15 |
** |
|
[15;19] |
2 |
1 |
1.25 |
|
3149 |
0.12 |
0.13 |
** |
|
[20;24] |
2 |
0.2 |
1 |
|
2430 |
0.10 |
-0.16 |
** |
|
[25;29] |
0 |
0 |
-1 |
|
1919 |
0.10 |
-0.18 |
** |
|
[30;34] |
5 |
0.36 |
2.21 |
|
2502 |
0.13 |
-0.11 |
** |
|
[35;39] |
7 |
0.19 |
0.10 |
|
3248 |
0.15 |
-0.15 |
** |
|
[40;44] |
20 |
0.19 |
0.02 |
|
4140 |
0.16 |
-0.03 |
|
|
[45;49] |
31 |
0.21 |
0.68 |
** |
3096 |
0.17 |
-0.12 |
** |
|
[50;54] |
73 |
0.18 |
0.32 |
** |
3705 |
0.18 |
-0.05 |
* |
|
[55;59] |
253 |
0.17 |
0.20 |
* |
6318 |
0.19 |
0.05 |
** |
|
[60;64] |
427 |
0.16 |
0.14 |
* |
5307 |
0.19 |
0.19 |
** |
|
[65;69] |
564 |
0.16 |
0.19 |
** |
3557 |
0.18 |
0.13 |
** |
|
[70;74] |
559 |
0.15 |
0.17 |
** |
2721 |
0.18 |
0.09 |
** |
|
[75;79] |
535 |
0.15 |
0.16 |
* |
1978 |
0.18 |
0.13 |
** |
|
80+ |
783 |
0.14 |
0.24 |
* |
2674 |
0.16 |
0.14 |
** |
|
Total |
3261 |
0.15 |
0.15 |
** |
61979 |
0.16 |
0.04 |
** |
*p<0.05 **p<0.01.
Discussion
Database analysis of a large closed population of type 2 diabetic patients, in a 4-year follow-up period, demonstrate specific oral health modifications: the dental extraction frequency exhibits an early and continuous high rate, despite regular dental checkups and scaling prophylaxis sessions. Over time the closed CPR population characteristics are in agreement with the general French population data: the CPR DT2 2012 population showed a 5.12% rate that compares to the at 4.7% rate of the 3.086 million French diabetic in the general population. Moreover, the deceased patients represent 18.82 % of the CPR DT2 population over 4 years which is an annual death rate of 4.7%. This is similar to the mortality rate of the diabetic patients in France [22].
Several studies have investigated the causes of death and mortality rates (MR) in diabetic populations [23]. Using data analysis, a recent comprehensive analysis of the MR and cause of death in a Korean population, with type 2 diabetes, showed that diabetic men had a higher mortality risk than diabetic women, which is connoted with our results in a French population [24]. Moreover, excess mortality, which was primarily contributed by cardiovascular and ischemic heart diseases, has been shown to be presumably indirectly related to periodontal disease and tooth loss. We detected a positive association between tooth loss and cardiovascular diseases and also found that the association differed depending on sex with male subjects being more prone to the disease [25].
Long term study on the natural history of periodontal disease and tooth loss over 40 years showed that smoking and calculus were associated with disease initiation and that calculus, plaque, and gingivitis were associated with loss of attachment and progression to advanced disease [26]. Evidence suggest that calculus removal, plaque control, and the control of gingivitis are essential in preventing disease progression, further loss of attachment and ultimately tooth loss. Diabetic patients undergo tooth loss at specific age ranges that appear to be on average 15 years later in 2016 as compared to 2012. Here, the studied population showed an increase for tooth extraction in the 40-44 and 55-59 age ranges in 2012, and then an increase in the 55-59 and 75-79 ranges in 2016. It appears that tooth loss in diabetic patients is not a continuous process but occurs at some specific age range that can be traced in this study in the mid-forties, mid-fifties and mid-seventies thus leading to a higher edentulous state than the normal population which for the extraction prevalence steadily increases with age. However, an increase frequency in periodontal treatment (scaling- prophylaxis session) precedes the tooth extraction age range suggesting that a periodontal awareness of the patients is present over time.
These data suggest that periodontal disease leading to tooth loss in diabetes is controlled but not definitively cured over this time-length, notwithstanding common dental prevention regimens. Therefore, the dental care sessions involving routine checkups and regular scaling prophylaxis sessions appear necessary and cannot be either spaced or discontinued [27]. Tooth loss in diabetes is the result of a peculiar infectious disease and the end stage of periodontitis; the multifactorial etiology of this disease involves species bacterial and also recognizes social determinants linked to nutrition and oral hygiene [28]. This appears unique compared to other infectious disease that usually can be cured through appropriate medical treatment.
In the dental field some analogy can be found with the recurrence of carious disease or the modification of its clinical presentation when fluoride prevention is discontinued. Further studies will try to find out the sequence of the extracted teeth (anterior or posterior) and find the annual rate of edentulism and if tooth loss could be linked to the level of control of the diabetes and whether some threshold levels for HbA1c levels correlate with tooth loss over time.
Acknowledgments
We thank data managers at CPRP for access to the database, Dr F Desideri, chief medical officer and P. Robin, CPRP director for their support.
Conflicts of Interest
None.
Funding
None.
Abbreviations
CPRP : Caisse de Prévoyance et de Retraite des Personnels
SNCF: Société Nationale des Chemins de Fer Français
Article Info
Article Type
Research ArticlePublication history
Received: Wed 04, Mar 2020Accepted: Fri 20, Mar 2020
Published: Tue 31, Mar 2020
Copyright
© 2023 Marie-Laurène Mayard-Pons. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDMC.2020.01.02
Author Info
Marie-Laurène Mayard-Pons Frédéric Rilliard Anne-Marie Musset Pierre Farge
Corresponding Author
Marie-Laurène Mayard-PonsMedical and Dental department, CPRP SNCF, Paris, France
Figures & Tables
Table 1: Populations 2012-2016.
|
|
2012 |
2016 |
|||||||||
|
|
n |
% of sample |
mean age (yrs.) |
SD |
Confidence Intervals 95% confident |
|
n |
% of sample |
mean age (yrs.) |
SD |
Confidence Intervals 95% confident |
|
All (A) |
533 378 |
100 |
46.33 |
26.42 |
[46.26;46.40] |
All (A) |
499 943 |
100 |
46.43 |
26.50 |
[46.36 ; 46.51] |
|
Female |
179 671 |
33.69 |
42.11 |
29.34 |
[41.97;42.25] |
Female |
163 908 |
32.79 |
41.71 |
29.28 |
[41.57 ; 41.85] |
|
Male |
353 707 |
66.31 |
48.44 |
24.57 |
[48.36;48.52] |
Male |
336 035 |
67.21 |
48.74 |
24.70 |
[48.66 ; 48.82] |
|
Non diabetic - free chronic disease (ND-FCD) |
377 207 |
70.72a |
39.48 |
24.38 |
[39.40;39.56] |
Non diabetic - free chronic disease (ND-FCD) |
383363 |
76.69a |
38.9 |
24.07 |
[38.83;38.98] |
|
Female |
132 997 |
35.26 |
35.52 |
26.63 |
[35.38;35.66] |
Female |
132 029 |
34.44 |
35.71 |
26.15 |
[35.57;35.85] |
|
Male |
244 210 |
64.74 |
41.63 |
22.78 |
[41.54;41.72] |
Male |
251 334 |
65.56 |
41.35 |
22.9 |
[41.26;41.44] |
|
Type 2 Diabetic (D) |
27 305 |
5.12b |
71 |
11.2 |
[69.87;71.13] |
Type 2 Diabetic (closed cohort D) |
22 096 |
4.42b |
72.61 |
10.75 |
[72.46 ; 72.75] |
|
Female |
6562 |
24.03 |
74 |
12.2 |
[73.74;74.34] |
Female |
5180 |
23.44 |
75.41 |
12.04 |
[75.08;75.74] |
|
Male |
20743 |
75.97 |
70 |
10.6 |
[69.87;70.16] |
Male |
16916 |
76.56 |
72.15 |
10.2 |
[72.00;72.31] |
|
Type 2 Diabetic mortality rate 2012-2016 |
5 139 |
18.82c |
82.08 |
9.4 |
[81.83 ; 82.34] |
Type 2 Diabetic lost to follow up 2012-2016 |
70 |
0.26 |
|
|
|
|
Female |
1341 |
26.09 |
86 |
8.37 |
[85.63;86.52] |
Female |
41 |
0.62 |
|
|
|
|
Male |
3798 |
73.91 |
80.7 |
9.33 |
[80.38;80.97] |
Male |
29 |
0.14 |
|
|
|
a % of sample: ND-FCD population represents % of all CPR population.
b % of sample: Type 2 diabetic population represents % of all CPR population.
c % of sample: Type 2 diabetic mortality rate represents % of 2012 Type 2 diabetic population.
Table 2: Ratio of teeth extractions and scaling-prophylaxis sessions among the two populations by age group in 2016 and change 2016/2012.
|
Populations 2016 |
Scaling prophylaxis sessions 2016 |
Tooth extractions 2016 |
||||||||||||||
|
DT2 |
ND-FCD |
DT2 |
ND-FCD |
|
DT2 |
NDFCD |
|
|||||||||
|
Age |
n |
n |
nb of scaling sessions |
ratio |
change 2016/ 2012 |
nb of scaling sessions |
ratio |
change 2016/ 2012 |
RR |
nb of tooth extractions |
ratio |
change 2016/ 2012 |
nb of tooth extractions |
ratio |
change 2016/ 2012 |
RR |
|
[0;9] |
0 |
54576 |
0 |
0 |
0 |
1901 |
0.03 |
-0.12** |
0.00 |
0 |
0 |
0 |
41 |
0.00 |
-0.97** |
0.00 |
|
[10;14] |
0 |
29242 |
0 |
0 |
0 |
4878 |
0.17 |
0.39** |
0.00 |
0 |
0 |
0 |
785 |
0.03 |
-0.74** |
0.00 |
|
[15;19] |
2 |
25293 |
0 |
0 |
-1 |
6164 |
0.24 |
0.27** |
0.00 |
2 |
1 |
0 |
329 |
0.01 |
-0.11 |
76.88 |
|
[20;24] |
10 |
24395 |
7 |
0.70 |
-0.13 |
7549 |
0.31 |
0.05** |
2.26 |
0 |
0 |
0 |
449 |
0 .02 |
-0 .19** |
0.00 |
|
[25;29] |
11 |
19628 |
1 |
0.09 |
-0.83* |
7156 |
0.36 |
0.12** |
0.25 |
0 |
0 |
-1 |
707 |
0.04 |
0.04 |
0.00 |
|
[30;34] |
14 |
19187 |
1 |
0.07 |
-0.61 |
7793 |
0.41 |
0.04* |
0.18 |
1 |
0.07 |
-0.04 |
872 |
0.05 |
-0.16** |
1.57 |
|
[35;39] |
36 |
22007 |
11 |
0.31 |
-0.36 |
10252 |
0.47 |
0.12** |
0.66 |
3 |
0.08 |
-0.11 |
1236 |
0.06 |
-0.09* |
1.48 |
|
[40;44] |
108 |
25420 |
50 |
0.46 |
-0.11 |
12252 |
0.48 |
0.26** |
0.96 |
12 |
0.11 |
-0.55 |
1727 |
0.07 |
-0.03 |
1.64 |
|
[45;49] |
147 |
17965 |
85 |
0.58 |
0.58** |
10178 |
0.57 |
0.31** |
1.02 |
15 |
0.10 |
-0.16 |
1671 |
0.09 |
-0.08* |
1.10 |
|
[50;54] |
401 |
20240 |
103 |
0.26 |
-0.23** |
8627 |
0.43 |
-0.02 |
0.60** |
65 |
0.16 |
0.13 |
2309 |
0.11 |
-0.12** |
1.42 |
|
[55;59] |
1511 |
33984 |
496 |
0.33 |
-0.01 |
17268 |
0.51 |
0.15** |
0.65** |
346 |
0.23 |
0.15 |
4814 |
0.14 |
-0 .07** |
1.62** |
|
[60;64] |
2704 |
28637 |
989 |
0.37 |
0.27** |
15853 |
0.55 |
0.48** |
0.66** |
579 |
0.21 |
0.20 |
4703 |
0.16 |
0.03 |
1.30** |
|
[65;69] |
3507 |
20077 |
1126 |
0.32 |
0.32** |
10229 |
0.51 |
0.54** |
0.63** |
636 |
0.18 |
-0.04 |
3564 |
0.18 |
0 .05 |
1.02 |
|
[70;74] |
3672 |
14803 |
1171 |
0.32 |
0.52** |
6859 |
0.46 |
0.49** |
0.69** |
770 |
0.21 |
0.15 |
2686 |
0.18 |
0 .00 |
1.16** |
|
[75;79] |
3590 |
10788 |
920 |
0.26 |
0.56** |
4331 |
0.40 |
0.57** |
0.64** |
808 |
0.23 |
0.27 |
2288 |
0.21 |
0 .06 |
1.06 |
|
80+ |
6383 |
17121 |
1112 |
0.17 |
0.51** |
4395 |
0.32 |
0.99** |
0.68** |
1134 |
0.18 |
0.11 |
3098 |
0.18 |
0.05 |
0.98 |
|
Total |
22096 |
383363 |
6072 |
0.27 |
0.26** |
135685 |
0.35 |
0.26** |
0.78** |
4371 |
0.20 |
0.13 |
31279 |
0.08 |
-0.13** |
2.42** |
NS : No statistical Significance *p<0,05 **p<0,01.
Table 3: Outpatient dental appointments into the two populations in 2016.
|
|
DT2 dental consultations |
NDFCD dental consultations |
||||||
|
|
2016 |
|
|
2016 |
|
|
||
|
Age |
nb of dental consultations |
ratio |
change 2016/2012 |
nb of dental consultations |
ratio |
change 2016/2012 |
||
|
[0;9] |
0 |
0 |
0 |
|
8505 |
0.16 |
0.18 |
** |
|
[10;14] |
0 |
0 |
0 |
|
6730 |
0.23 |
0.15 |
** |
|
[15;19] |
2 |
1 |
1.25 |
|
3149 |
0.12 |
0.13 |
** |
|
[20;24] |
2 |
0.2 |
1 |
|
2430 |
0.10 |
-0.16 |
** |
|
[25;29] |
0 |
0 |
-1 |
|
1919 |
0.10 |
-0.18 |
** |
|
[30;34] |
5 |
0.36 |
2.21 |
|
2502 |
0.13 |
-0.11 |
** |
|
[35;39] |
7 |
0.19 |
0.10 |
|
3248 |
0.15 |
-0.15 |
** |
|
[40;44] |
20 |
0.19 |
0.02 |
|
4140 |
0.16 |
-0.03 |
|
|
[45;49] |
31 |
0.21 |
0.68 |
** |
3096 |
0.17 |
-0.12 |
** |
|
[50;54] |
73 |
0.18 |
0.32 |
** |
3705 |
0.18 |
-0.05 |
* |
|
[55;59] |
253 |
0.17 |
0.20 |
* |
6318 |
0.19 |
0.05 |
** |
|
[60;64] |
427 |
0.16 |
0.14 |
* |
5307 |
0.19 |
0.19 |
** |
|
[65;69] |
564 |
0.16 |
0.19 |
** |
3557 |
0.18 |
0.13 |
** |
|
[70;74] |
559 |
0.15 |
0.17 |
** |
2721 |
0.18 |
0.09 |
** |
|
[75;79] |
535 |
0.15 |
0.16 |
* |
1978 |
0.18 |
0.13 |
** |
|
80+ |
783 |
0.14 |
0.24 |
* |
2674 |
0.16 |
0.14 |
** |
|
Total |
3261 |
0.15 |
0.15 |
** |
61979 |
0.16 |
0.04 |
** |
*p<0.05 **p<0.01.
References
- Nazir MA, AlGhamdi L, AlKadi M, AlBeajan N, AlRashoudi L et al. (2018) The burden of Diabetes, Its Oral Complications and Their Prevention and Management. Open Access Maced J Med Sci 6: 1545-1553. [Crossref]
- Löe H (1993) Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care 16: 329-334. [Crossref]
- Centers for Disease Control and Prevention. National diabetes statistics report (2017) Atlanta, GA: Centers for Disease Control and Prevention.
- Lalla E, Papapanou PN (2011) Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol 7: 738-748. [Crossref]
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ et al. (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378: 31-40. [Crossref]
- Casanova L, Hughes FJ, Preshaw PM (2014) Diabetes and periodontal disease: a two-way relationship. Br Dent J 217: 433-437. [Crossref]
- Kaur G, Mohindra K, Singla S (2017) Autoimmunity-Basics and link with periodontal disease. Autoimmun Rev 16: 64-71. [Crossref]
- Graves DT, Corrêa JD, Silva TA (2019) The Oral Microbiota Is Modified by Systemic Diseases. J Dent Res 98: 148-156. [Crossref]
- Simpson TC, Weldon JC, Worthington HV, Needleman I, Wild SH et al. (2015) Treatment of periodontal disease for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev 11: CD004714. [Crossref]
- Indurkar MS, Maurya AS, Indurkar S (2016) Oral Manifestations of Diabetes. Clin Diabetes 34: 54-57. [Crossref]
- Kudiyirickal MG, Pappachan JM (2015) Diabetes mellitus and oral health. Endocrine 49: 27-34. [Crossref]
- Li Q, Hao S, Fang J, Xie J, Kong XH et al. (2015) Effect of non-surgical periodontal treatment on glycemic control of patients with diabetes: a meta-analysis of randomized controlled trials. Trials 16: 291. [Crossref]
- Mizuno H, Ekuni D, Maruyama T, Kataoka K, Yoneda T et al. (2017) The effects of non-surgical periodontal treatment on glycemic control, oxidative stress balance and quality of life in patients with type 2 diabetes: A randomized clinical trial. PLoS One 12: e0188171. [Crossref]
- Artese HPC, Foz AM, Rabelo Mde S, Gomes GH, Orlandi M et al. (2015) Periodontal therapy and systemic inflammation in type 2 diabetes mellitus: a meta-analysis. PLoS One 10: e0128344. [Crossref]
- D'Aiuto F, Gable D, Syed Z, Allen Y, Wanyonyi KL et al. (2017) Evidence summary: The relationship between oral diseases and diabetes. Br Dent J 222: 944-948. [Crossref]
- Lund Håheim L, Rønningen KS, Enersen M, Olsen (2017) The Predictive Role of Tooth Extractions, Oral Infections, and hs-C-Reactive Protein for Mortality in Individuals with and without Diabetes: A Prospective Cohort Study of a 121/2-Year Follow-Up. J Diabetes Res 2017: 12.
- Peng CH, Yang YS, Chan KC, Kornelius E, Chiou JY et al. (2017) Periodontal Treatment and the Risks of Cardiovascular Disease in Patients with Type 2 Diabetes: A Retrospective Cohort Study. Intern Med 56: 1015-1021. [Crossref]
- Winning L, Patterson CC, Neville CE, Kee F, Linde GJ (2017) Periodontitis and incident type 2 diabetes: a prospective cohort study. J Clin Periodontol 44: 266-274. [Crossref]
- Patel MH, Kumar JV, Moss ME (2013) Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey,2003-2004. J Am Dent Assoc 144: 478-485. [Crossref]
- Liljestrand JM, Havulinna AS, Paju S, Männistö S, Salomaa V et al. (2015) Missing Teeth Predict Incident Cardiovascular Events, Diabetes, and Death. J Dent Res 94: 1055-1062. [Crossref]
- Mayard Pons ML, Rilliard F, Libersa JC, Musset AM, Farge P (2015) Database analysis of a French type 2 diabetic population shows a specific age pattern of tooth extractions and correlates health care utilization. J Diabetes Complications 29: 993-997. [Crossref]
- Mandereau Bruno L, Fagot Campagna A, Rey G, Piffaretti C, Antero Jacquemin J et al. (2016) Évolution de la mortalité et de la surmortalité à 5 ans des personnes diabétiques traitées pharmacologiquement en France métropolitaine : comparaison des cohortes Entred 2001 et Entred 2007. Bull Epidémiol Hebd 37-38: 668-675.
- Tancredi M, Rosengren A, Svensson AM, Kosiborod M, Pivodic A et al. (2015) Excess Mortality Among Persons with Type 2 Diabetes. N Engl J Med 373: 1720-1732. [Crossref]
- Kang YM, Kim YJ, Park JY, Lee WJ, Jung CH (2016) Mortality and causes of death in a national sample of type 2 diabetic patients in Korea from 2002 to 2013. Cardiovasc Diabetol 15: 131. [Crossref]
- Asai K, Yamori M, Yamazaki T, Yamaquchi A, Takahashi K et al. (2015) Tooth loss and atherosclerosis: the Nagahama Study. J Dent Res 94: 52S-58S. [Crossref]
- Ramseier CA, Anerud A, Dulac M, Lulic M, Cullinan MP et al. (2017) Natural history of periodontitis: Disease progression and tooth loss over 40 years. J Clin Periodontol 44: 1182-1191. [Crossref]
- Jepsen S, Blanco J, Buchalla W, Carvalho JC, Dietrich T et al. (2017) Prevention and control of dental caries and periodontal diseases at individual and population level: consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 18: S85-S93. [Crossref]
- Valente MIB, Vettore MV (2018) Contextual and individual determinants of periodontal disease: Multilevel analysis based on Andersen's model. Community Dent Oral Epidemiol 46: 161-168. [Crossref]
