Urine Output Measurement by a Novel Electronic Urinometer is much more Accurate than by Conventional Urinometer
A B S T R A C T
Introduction: Assessment of urine output in hospitalized patients or those undergoing complex surgery is essential for preventing Acute Kidney Injury and increased mortality. Currently, measurements of urine output are made by visually inspecting the volume of urine that accumulates in a bag attached to a catheter which resides in the bladder by way of a manual urinometer. Several electronic urinometers have been tested but have not been clinically proven or accepted. We report preliminary results of a novel Electronic Urinometer (EU) and compared its accuracy to a conventional Manual Urinometer (MU).
Methods: The study included 22 consecutive ICU patients whose urine output was collected with a foley catheter. Urine output was measured for all patients by EU as well as by MU. Both measurements were compared to analysis of the volume in a Graduated Cylinder (GC).
Results: The EU was highly accurate in measurement of both urine volume and urine flow with an average deviation from GC 4 ± 3.0% vs 17 ± 23% for the MU (P<0.01).
Conclusion: This study showed that measuring urine output in ICU patients by an EU is more accurate than conventional MU.
Keywords
Urine output, vital signs, monitoring
Introduction
Urine output is an essential vital sign that is monitored in patients undergoing complex surgery, in hospitalized patients that require careful assessment of their fluid status as well as the vast majority of patients in the Intensive Care Unit (ICU). Flow rates below 0.5 cc/kg/hr are associated with the development of Acute Kidney Injury (AKI) and poor outcomes. Currently, urine output is measured by a manual urinometer: Anesthesiologists in the operating room and the nursing staff in the ICU and hospital wards record the urine output collected via a foley catheter by visually inspecting the volume of urine in a collection bag once every hour. In contrast, all other vital signs (i.e., blood pressure and heart rate, oxygenation, respiratory rate, temperature) are monitored by continuous recording and digital display [1].
Use of an electronic continuous urine output monitoring device may increase measurement accuracy, save medical staff time, and enable early diagnosis of impending AKI and circulatory failure [2]. Several attempts to develop an electronic urinometer have been made, but none have been clinically accepted to date. We describe a novel electronic urinometer, allows for accurate, continues real-time measurement of urine output. We compared accuracy of the conventional Manual Urinometer (MU) to the Electronic Urinometer (EU).
Methods
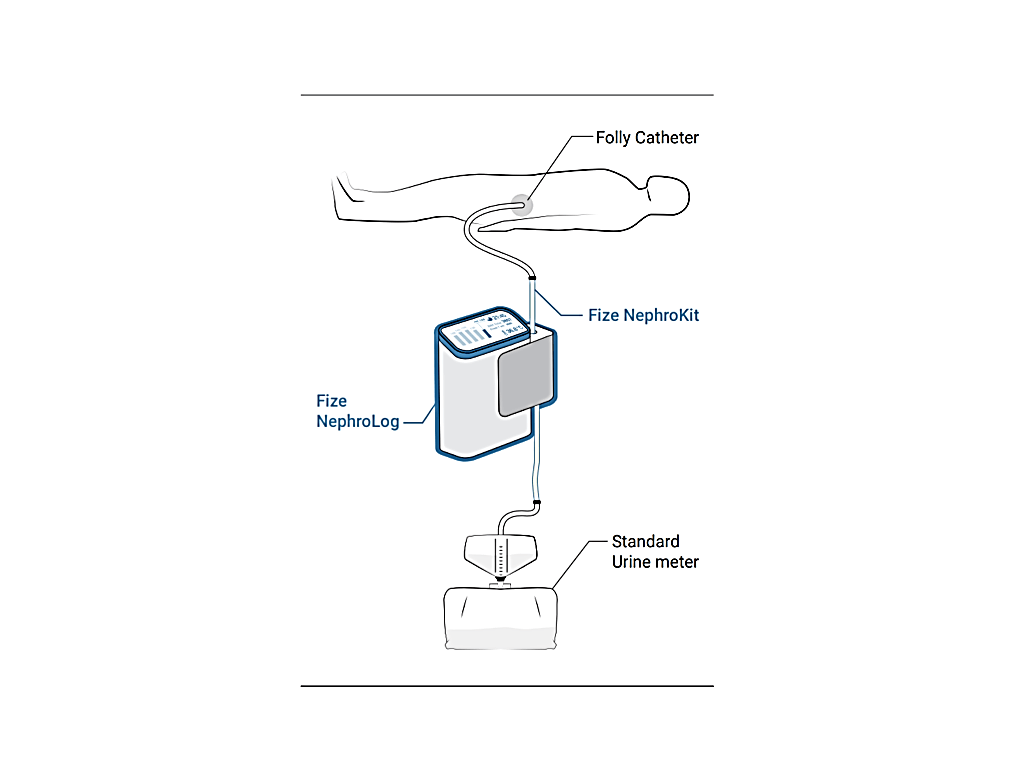
We tested a working prototype of an electronic urinometer (NephroLog, Fize Research Ltd), capable of measuring microliter resolution urine flow rates independent of the urine constitution. We measured urine flow and total output in 22 consecutive ICU patients. The EU was connected to the patient’s foley catheter and the MU was connected to a tube exiting the EU, hence allowing urine output measuring by both methods in tandem (Figure 1). The urine volume collected by the drainage bag of the MU was measured by a Graduated Cylinder (GC). This measurement served as the gold standard. The ICU staff measured the urine output of these patients on an hourly basis using the MU. The data collected by our EU was not available to the ICU team. The study protocol was approved by our institution review board.
Figure 1: Electronic Urinomer (Fize Research Ltd).
Statistical Analysis
Data are given as mean ± SD. Comparisons between two experimental groups were made by Student’s t test (two- tailed) after verification of normality. P values of ≤0.05 were considered statistically significant.Bland Altman plots were constructed in order to assess levels of agreement, respectively mean bias ± 2SD. Linear regression was used in order to explore possible existence of proportional bias.
Results
Of 22 patients 33 measurements were obtained. The average time-length of each measurement was 7.3 hours, and the total measurement time was 242 hours. Since both EU and MU were connected in tandem, urine exiting the patient foley catheter passed through the EU and then collected by the MU. Therefore, the same urine volume passed through both systems, over the same time length. As shown in (Figure 2) compare to the (GC) measurement- the EU measurement was much more accurate than the MU measurement. the average deviation from GC measurement was 4 ± 3.0% for the MU and 17 ± 23% for the MU (P<0.01).
Figure 2: Bland Altman plots Accuracy of the Electronic Urinometer (EU) and the Manual Urinometer (MU), each compared to the Graduated Cylinder (GC).
Discussion
This study demonstrated that the EU provides a significantly more accurate assessment of urine output than the conventional MU when both are compared to a gold standard measurement by the GC.Different types of EU’s using different techniques, have been tested by other groups who compared their accuracy to MU. They too were able to demonstrate that an EU can be more accurate [3, 4]. However, in their studies, patient populations were divided into 2 discreet groups: the first group was allocated to EU and second group to MU. Our study was unique, in having the total output for all patients measured both in the EU and the MU, enabling a direct comparison between the two methods in relation to the recorded volume in one graduated cylinder.
In summary, urine output measurement in Intensive Care Unit patients by the Fize EU is more accurate than standard measures with a MU. Utilizing an EU has the potential to improve accuracy of this vital measurement, decrease manual labor and provide digital data inputs into today’s modern electronic medical record (EMR) systems. Automating and digitizing urine output measurement, as suggested by others, has the potential to impact clinical decision making and patient outcomes by enabling early recognition of Acute Kidney Injury, hemodynamic instability and overall mortality [5-7]. Further studies with this novel device are warranted.
Acknowledgements
David Rott is a medical consultant for Fize Research Ltd.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 02, May 2020Accepted: Mon 18, May 2020
Published: Fri 26, Jun 2020
Copyright
© 2023 David Rott. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.03.04
Author Info
David Rott Ilan Hay Robert Klempfner
Corresponding Author
David RottThe Leviev Heart Centre, The Chaim Sheba Medical Centre, Tel Hashomer, Israel
Figures & Tables

References
- Curley FJ and Smyrnios NA (1990) Routine monitoring of Critically Ill Patients. J Int Care Med 5: 153-174.
- Grover C, Barney K (2004) Operating safely in surgery and critical care with perioperative automation. J Healthc Inf Manag 18: 56-61. [Crossref]
- Hersch M, Einav S, Izbicki G (2009) Accuracy and ease of use of a novel electronic urine output monitoring device compared with standard manual urinometer in the intensive care unit. J Crit Care 24: 629.e13-629.e17. [Crossref]
- Eklund A, Slettengren M, van der Linden J (2015) Performance and user evaluation of a novel capacitance-based automatic urinometer compared with a manual standard urinometer after elective cardiac surgery. Crit Care 19: 173. [Crossref]
- Shamir MY, Kaplan L, Marans RS, Willner D, Klein Y (2011) Urine flow is a novel hemodynamic monitoring tool for the detection of hypovolemia. Anesth Analg 112: 593-596. [Crossref]
- Klein Y, Grinstein M, Cohn SM, Silverman J, Klein M et al. (2012) Minute-to-minute urine flow rate variability: a new renal physiology variable. Anesth Analg 115: 843-847. [Crossref]
- Otero A, Cardinal-Fernández P, Rojas Y, Nin N, Martínez-Caro L et al. (2014) On the minute by minute variations of urine output: a study in a porcine model. J Nephrol 27: 45-50. [Crossref]
