Venous Thromboembolic Disease Among the Lebanese Population: A Retrospective Observational Study
A B S T R A C T
Aims: To assess the characteristics and risk factors for patients presenting with venous thromboembolic disease (VTE) in Lebanon.
Methods: This was a retrospective, multicenter study that was conducted between the years of 2018-2019 in Lebanon. All medical charts with positive findings for VTE were included. Data on baseline characteristics, risk factors, signs and symptoms of disease, diagnostic findings, treatment, readmission and mortality rates at 1 year were collected.
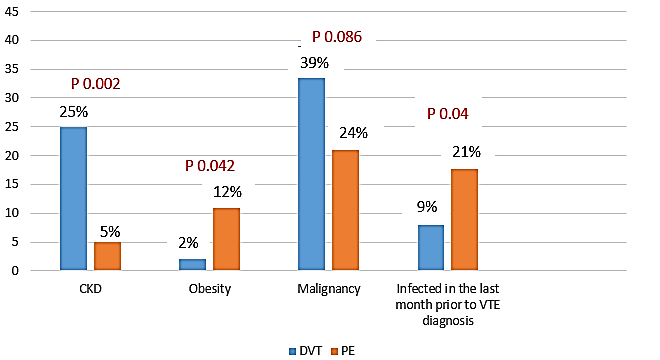
Results: 1500 charts were reviewed. We included 132 confirmed diagnosis with deep vein thrombosis (DVT) or pulmonary embolism (PE). Out of 132 patients 43% were diagnosed with DVT, 42% with PE and 15% having both DVT and PE. Mean age was 61 years. Current smokers were 36%. Coronary artery disease was found in 19.5%, diabetes in 11%, atrial fibrillation in 10.5% and malignancy in 30% of the cases. Readmission rate within 1 year was 35%. In hospital mortality was 13% and one-year mortality was 22%. Characteristics of patients diagnosed with DVT vs patients diagnosed with PE were comparable. However, we noted that chronic kidney disease was more prevalent in patients with DVT than in patients with PE (25% vs 5% respectively; p- 0.002). Obesity was found less in patients with DVT than in patients with PE (2% vs 12% respectively; p-0.042). Patients with malignancy were diagnosed more with DVTs than with PE; however, the p-value was not statistically significant (39% vs 24% respectively; p-0.086). Patients with recent infection in the prior month of diagnosis was noted to be a predisposing factor for PE than for DVT (21% vs 9% respectively; p-0.04). Mortality within one year was significantly associated with male gender (p-0.009) and having a diagnosis of DVT+PE (p-0.005).
Conclusion: Our study revealed a high burden of VTE in Lebanon. Malignancy and prior infection were a predisposing factor for VTE. The readmission rate and the one-year mortality were significantly elevated. Mortality was significantly associated with the diagnosis of combined DVT and PE at the same time.
Keywords
VTE, DVT, PE, risk factors, morbidity, mortality
Background
Venous thromboembolism (VTE) is the third most frequent acute cardiovascular syndrome behind myocardial infarction and stroke [1]. Deep venous thrombosis (DVT) and pulmonary embolism (PE) are the clinical presentation of VTE. Annual incidence rates for DVT range from 53 to 162 per 100 000 population whereas 39 to 115 per 100,000 population for PE [2, 3]. Patients with VTE have increased morbidity and mortality related to cancer, surgical procedures, and other medical conditions [4]. The 12-month mortality rate of DVT varied between 2.9% in the pooled data from Germany, Switzerland or Austria and 15.4% in Italy. The 12 months mortality rate for PE was 5.2% in France, 16.8% in Italy, 9.1% in Spain and 2.6% in the UK [5]. Furthermore, the mortality rate differed between patients with active cancer and those without (42.9% vs 4.7%) [6]. Multiple risk factors are associated with thromboembolism. Major trauma, surgery, cancer, estrogen-containing oral contraceptive agents, hormone replacement therapy in postmenopausal women, infection, obesity and genetics play a major role in the pathogenesis of thromboembolism. Since the pathogenesis of thromboembolism is multifactorial and some of risk factors are modifiable plus the high burden of morbidity and mortality, we decided to conduct a retrospective multicenter study to evaluate the factors among Lebanese population for better understanding VTE disease in order to improve morbidity and mortality in Lebanon.
Methods
This was a retrospective, multicenter study that was conducted between the years of 2018 to 2019 in two academic medical centers in Lebanon after gaining approval of the Institutional Review Board of both institutions, Rafik Hariri University Hospital and Lebanese American University Medical Center. Data was retrieved for all patients who underwent venous doppler ultrasound of lower extremities and CT angiography of the chest. All medical charts with positive results for DVT or PE were included. Out of 1500 medical chart reviewed, 132 were noted to have either DVT, PE or both. Data on baseline characteristics, risk factors, signs and symptoms of disease, diagnostic findings, treatment, readmission and mortality rate at 1 year were collected using case report forms. Data were then analysed and variables were compared in patients with DVT versus patients with PE with or without DVT.
Statistical Analysis
Data was entered and analysed using the SPSS IBM software, version 26. Descriptive statistics were used to report all participants’ responses. Continuous variables were described using mean and standard deviation. Categorical variables were described using frequencies. Variables were compared in patients with DVT versus patients with PE with or without DVT. Mortality was evaluated as a dependent variable. The association between categorical variables were evaluated using Pearson x2 test or Fisher’s exact test where the expected cell count < 5. Binary logistic regressions were performed to identify factors that affect dichotomous dependent variables using enter method. Results are assumed to be significant when p < 0.05 for all statistical analysis. No formal power calculation was conducted.
Table 1: The basic characteristics of patients with DVT vs patients with PE during index admission.
|
Variable |
Patients with DVT n = 57 |
Patients with PE n = 75 |
P-Value |
|
Hospital RHUH LAUMCRH |
33 (58) 24 (42) |
47 (63.7) 28 (37.3) |
0.594
|
|
Gender Male Female |
29 (50.9) 28 (49.1) |
36 (48) 39 (52) |
0.861 |
|
Age (Mean in years +/- SD) |
64.6 (+/- 14.9) |
59.7 (+/-17.8) |
0.093 |
|
Smoking Non-smoker Current Smoker |
28 (49.1) 14 (24.6) |
31 (41.3) 11 (14.7) |
0.286 0.230 |
|
Alcohol Non-alcoholic Current |
48 (84.2) 5 (8.8) |
67 (89.3) 7 (9.3) |
0.438 1.000 |
|
Symptoms and Signs Dyspnea Chest pain Cough Hemoptysis Pain in the affected extremity Swelling and tenderness in the affected extremity |
12 (21.1) 4 (7.0) 5 (8.8) 1 (1.8) 29 (50.9) 42 (75.0) |
57 (77.0) 21 (28.4) 21 (28.4) 4 (5.4) 12 (16.2) 10 (13.5) |
0.000 0.002 0.007 0.387 0.000 0.000 |
|
Imaging Findings Cardiomegaly Pulmonary edema Atelectasis Pleural effusion |
11 (19.3) 8 (14.0) 17 (29.8) 15 (26.3) |
34 (46.6) 12 (16.2) 27 (36.5) 28 (37.8) |
0.001 0.731 0.423 0.164 |
|
ECG Findings Sinus tachycardia RBBB ST-T Changes TWIs in inferior + anteroseptal leads |
15 (26.3) 4 (7.0) 2 (3.5) 3 (5.3) |
27 (36.5) 3 (4.1) 3 (4.1) 0 (0) |
0.216 0.468 1.000 0.080 |
Results
A total of 1500 charts were reviewed. We confirmed the diagnosis of PE and or DVT in 132 cases. Out of 132 cases studied 43% were diagnosed with DVT, 42% with PE and 15% having both DVT and PE. Mean age was 61 years. The prevalence of disease was almost the same between males and females (51 vs 49). Current smokers were 36%. Coronary artery disease was found in 19.5% of patients, diabetes in 11%, atrial fibrillation in 10.5% and malignancy in 30% of the cases. In the last three months prior to VTE diagnosis, 26% of the patients were hospitalized for different reasons 36% had infection and 21% had recent surgeries. Bed rest for more than 48 hours was detected in 29% of the cases. Dyspnea was the most common symptom detected in 52% of the cases, followed by swelling and tenderness in the affected extremity, in addition to chest pain and palpitations (Table 1). The most common finding on CXR was cardiomegaly in 34% followed by atelectasis in 33.3% and pleural effusion in 32.6%. Sinus tachycardia was a common finding on ECG. In total 53% of the cases required oxygen during admission. Out of the total patients 15% were intubated and 6% required BiPAP. In hospitalized patients 69% were treated with low molecular weight heparin and 39% were treated with heparin. Bleeding was detected in 12% of the cases of whom 6% required transfusion. CVA was noted in 1.5% of the patients. The readmission rate at 1 year was 35% and the one-year mortality was 22% (Figure 2).
Characteristics for patients with DVT vs patients with PE were comparable (Figure 1). However chronic kidney disease was noted more in patients with DVT than in patients with PE (25% vs 5% respectively; p- 0.002). Obesity was found less in patients with DVT than in patients with PE (2% vs 12% respectively; p-0.042). Patients with malignancy were diagnosed more with DVTs than PE, however the p-value was not statistically significant (39% vs 24% respectively; p-0.086). Being infected in the prior month before the diagnosis of VTE was a predisposing factor for PE than for DVT (21% vs 9% respectively; p-0.04). Patients with PE with or without DVT were more likely to be intubated than patients with DVT (22% vs 7%; p-0.026). Readmission rate within 1 year was 39% for patients with DVT vs 32% for patient with PE (p-0.465). Mortality within 1 year was higher in the PE vs DVT but it does not reach statistically significant value. (25% vs 17.5%; p-0.284) (Figure 2). Mortality within one year was significantly associated with male gender (p-0.009) and having a diagnosis of DVT with PE (p-0.005).
Figure 1: Comparison of patients with DVT and PE during the index admission.
Figure 2: Readmission rates and mortality within one year for patients with DVT vs PE from the index admission.
Discussion
The findings of this study highlighted the multiple risk factors that predispose patients to DVT or PE. These risk factors could be modified and could be a screening method to prevent this life-threatening condition. Moreover, it demonstrated the high rate of morbidity and mortality associated with such diagnosis. Screening for VTE in patients with malignancy may decrease the burden of VTE and improve outcome of these patients. Trying to decrease the burden of infections may also decrease the incidence of VTE. When we compare our data to a previous study that was done in Lebanon evaluating the risk factors associated with thromboembolism we noted similar findings with overweight, recent surgery, malignancy, and infection which all were associated with increased risk of VTE. Moreover, thrombophilia that was not studied in our paper was the second most implicating factor among Lebanese population [7]. These findings highlight the importance of risk factor modification to decrease the burden of this disease.
The one-year readmission rate for DVT patients studied in our paper was 39%, and 32% for patients with PE whereas the one-year readmission rates for DVT or PE patients in Europe were 5.3% for primary diagnosis [8]. Mortality within one year was 17.5% among our DVT patients whereas it is 7.3% for DVT in Europe. The mortality rate differed among countries, 6.7% in France, 2.9% in DACH countries (Austria, Germany and Switzerland), 15.4% in Italy, 6.1% in Spain, and 3.1% in the UK. Moreover, mortality was 43.0% in patients with active cancer and 3.8% in patients without active cancer [9]. One-year mortality was 25% among our PE patients whereas it was 8.1% for PE in Europe, ranging from 1.4% in Germany, Switzerland, and Austria to 16.8% in Italy. Mortality differed between patients with active cancer (42.7%) and those without (4.7%) [10]. Our data showed that the readmission rates for both DVT and PE and one-year mortality was significantly higher in our population in comparison with European countries. This implies that we have to set national guidelines in this field to target modifiable risk factors in order to decrease morbidity and mortality in such patients.
Limitations
There are multiple limitations in our study. First it is a retrospective study that will limit data collection to whatever was available and requested by physicians. Second this study looked only on patients admitted with the diagnosis of VTE we did not report any data on patients treated in the outpatient setting. However, the finding of our study highlighted important actions to be taken to improve the burden of disease.
Conclusion
Our study revealed a high burden of VTE in Lebanon with high morbidity and mortality. Malignancies and prior infection were an important predisposing risk factor for VTE. Measures that target risk factors, screening for malignancy, prophylaxis pre and post-surgery, and early mobilization, may decrease such burden.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 13, Jun 2020Accepted: Thu 25, Jun 2020
Published: Thu 06, Aug 2020
Copyright
© 2023 Souzan Tatari. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.HCS.2020.01.04
Author Info
Souzan Tatari Hussein Kordi Ali Allouch Ali El-Sayed Nibal Chamoun Elsy Ramia Samer Kabbani
Corresponding Author
Souzan TatariRafik Hariri University Hospital, Jnah, Beirut, Lebanon
Figures & Tables
Table 1: The basic characteristics of patients with DVT vs patients with PE during index admission.
|
Variable |
Patients with DVT n = 57 |
Patients with PE n = 75 |
P-Value |
|
Hospital RHUH LAUMCRH |
33 (58) 24 (42) |
47 (63.7) 28 (37.3) |
0.594
|
|
Gender Male Female |
29 (50.9) 28 (49.1) |
36 (48) 39 (52) |
0.861 |
|
Age (Mean in years +/- SD) |
64.6 (+/- 14.9) |
59.7 (+/-17.8) |
0.093 |
|
Smoking Non-smoker Current Smoker |
28 (49.1) 14 (24.6) |
31 (41.3) 11 (14.7) |
0.286 0.230 |
|
Alcohol Non-alcoholic Current |
48 (84.2) 5 (8.8) |
67 (89.3) 7 (9.3) |
0.438 1.000 |
|
Symptoms and Signs Dyspnea Chest pain Cough Hemoptysis Pain in the affected extremity Swelling and tenderness in the affected extremity |
12 (21.1) 4 (7.0) 5 (8.8) 1 (1.8) 29 (50.9) 42 (75.0) |
57 (77.0) 21 (28.4) 21 (28.4) 4 (5.4) 12 (16.2) 10 (13.5) |
0.000 0.002 0.007 0.387 0.000 0.000 |
|
Imaging Findings Cardiomegaly Pulmonary edema Atelectasis Pleural effusion |
11 (19.3) 8 (14.0) 17 (29.8) 15 (26.3) |
34 (46.6) 12 (16.2) 27 (36.5) 28 (37.8) |
0.001 0.731 0.423 0.164 |
|
ECG Findings Sinus tachycardia RBBB ST-T Changes TWIs in inferior + anteroseptal leads |
15 (26.3) 4 (7.0) 2 (3.5) 3 (5.3) |
27 (36.5) 3 (4.1) 3 (4.1) 0 (0) |
0.216 0.468 1.000 0.080 |

References
- Raskob GE, Angchaisuksiri P, Blanco AN, Buller H, Gallus A et al. (2014) Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol 34: 2363-2371. [Crossref]
- Wendelboe AM, Raskob GE (2016) Global burden of thrombosis: epidemiologic aspects. Circ Res 118: 1340-1347. [Crossref]
- Keller K, Hobohm L, Ebner M, Kresoja K, Munzel T et al. (2020) Trends in thrombolytic treatment and outcomes of acute pulmonary embolism in Germany. Eur Heart J 41: 522-529. [Crossref]
- Spencer FA, Emery C, Lessard D, Anderson F, Emani S et al. (2006) The Worcester Venous Thromboembolism study: a population-based study of the clinical epidemiology of venous thromboembolism. J Gen Intern Med 21: 722-777. [Crossref]
- Chuang L, Gumbs P, van Hout B, Agnelli G, Kroep S et al. (2019) Health-related quality of life and mortality in patients with pulmonary embolism: a prospective cohort study in seven European countries. Qual Life Res 28: 2111-2124. [Crossref]
- Monreal M, Agnelli G, Chuang LH, Cohen AT, Gumbs PD et al. (2019) Deep Vein Thrombosis in Europe-Health-Related Quality of Life and Mortality. Clin Appl Thromb Hemost 25: 1076029619883946. [Crossref]
- Rizk S, Hammoud N, Zein S, Awada S, Rachidi S et al. (2018) Evaluation of Risk Factors Associated with Venous Thromboembolism in the Lebanese Population. Cardiology Angiology 7: 1-12.
- Friedman RJ (2010) Simplifying thromboprophylaxis could improve outcomes in orthopedics surgery. Thrombosis 2010: 108049. [Crossref]
- Monreal M, Agnelli G, Chuang LH, Cohen AT, Gumbs PD et al. (2019) Deep Vein Thrombosis in Europe-Health-Related Quality of Life and Mortality. Clin Appl Thromb Hemost 25: 1076029619883946. [Crossref]
- Chuang LH, Gumbs P, van Hout B, Agnelli G, Kroep S et al. (2019) Health‑related quality of life and mortality in patients with pulmonary embolism: a prospective cohort study in seven European countries. Qual Life Res 28: 2111-2124. [Crossref]
